Discussion
Discussion
Genetic testing for Huntington’s disease
Last updated Jan. 15, 2025, by Lindsey Shapiro, PhD

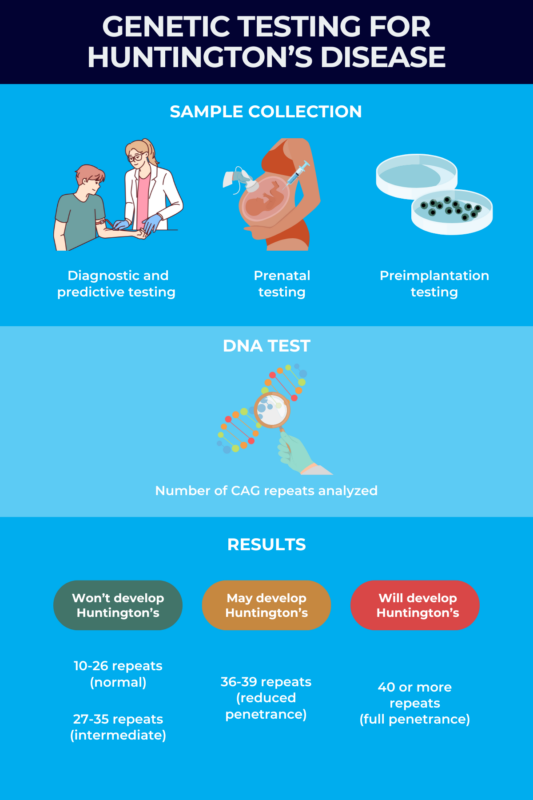
Genetic testing, which is when a person’s DNA is screened for disease-related mutations, plays a key role in determining whether a person has or will develop Huntington’s disease.
Huntington’s disease is a neurodegenerative condition caused by mutations in the HTT gene. Deciding whether to do genetic testing is a highly personal decision and can have significant emotional consequences. It is usually recommended that time is taken to carefully consider whether genetic testing is the right choice; the decision should not be rushed.
It’s important to understand how genetic testing works, what it can offer, and its potential limitations before making a choice.
How does genetic testing work?
Huntington’s disease is a condition that typically runs in families. It’s caused by a genetic mutation in the HTT gene called a CAG trinucleotide repeat expansion. The mutation has a section of DNA where three DNA building blocks (nucleotides) — a cytosine (C) , an adenine (A), and a guanine (G) — are repeated too many times.
While the CAG trio is normally repeated 10-35 times in the HTT gene, a greater number of repeats causes the production of an abnormally long huntingtin protein, which can be toxic to nerve cells and lead to Huntington’s disease symptoms.
Every person inherits two copies of the HTT gene, one from their mother and one from their father. Having a Huntington’s-causing mutation in only one gene copy is enough for the disease to manifest. This also means that if a person with Huntington’s has a child, there’s a 50% chance that the child will inherit the disease-causing mutation and develop the disease.
Genetic testing is the most definitive way to establish a Huntington’s disease diagnosis. Basically, genetic testing for Huntington’s disease screens the DNA to determine the number of CAG repeats present in each copy of the HTT gene.
- Twenty-six or fewer CAG repeats are considered normal and not associated with a risk of Huntington’s.
- Twenty-seven to 35 CAG repeats are considered an intermediate result, meaning the person will not develop Huntington’s, but any children they have may inherit a longer repeat expansion that causes the disease. This is because 27-39 CAG repeats are considered unstable, and can be expanded when transmitted to the offspring, most often through the father.
- Thirty-six to 39 CAG repeats, classified as reduced penetrance, cannot reliably predict whether a person will develop Huntington’s — some people will develop symptoms and some won’t. Because of CAG repeat instability, even if someone does not develop symptoms, it is still possible to pass the disease on to any future children.
- Forty or more CAG repeats, called full penetrance, means it is essentially certain Huntington’s will develop at some point.
For those with a positive Huntington’s test, the number of repeats can also affect how early the disease emerges. In general, more CAG repeats are associated with an earlier disease onset, although this factor alone cannot entirely predict how the disease will develop.
Different types of genetic tests
There are a few different types of genetic tests that might be used to screen for Huntington’s. They all involve taking a fluid or tissue sample and screening the DNA for disease-causing mutations. Which test is used depends on the age at the time of testing and whether or not a person has Huntington’s disease symptoms.
Prenatal and preimplantation testing
If you have Huntington’s or a family history of the disease and want to have children, you might consider prenatal testing to evaluate whether the child will develop Huntington’s. If a woman is already pregnant, the fetus can be tested for Huntington’s in a couple different ways.
- Chorionic villus sampling is usually done during weeks 10-13 of pregnancy. It involves taking a small sample of tissue from the placenta, which contains fetal cells and DNA, directly through the cervix or by inserting a thin needle through the abdomen.
- Amniocentesis is usually done between 15 and 20 weeks of pregnancy. It involves inserting a thin needle into the abdomen to collect fetal cells and DNA by taking a sample of the fluid that surrounds and protects a baby in the womb.
Preimplantation genetic testing (PGT) is an option for families who want to make sure their children will be negative for Huntington’s-causing mutations prior to pregnancy.
This type of testing is used during the process of in vitro fertilization, or IVF, which involves collecting reproductive cells from each parent, combining them in a laboratory setting, and implanting the resulting embryo back into the mother’s uterus. Preimplantation testing screens embryos for Huntington’s-causing mutations before they’re implanted. Only embryos testing negative are implanted.
In some cases, parents opting for prenatal testing or PGT may not know — and may not wish to know — their own genetic status. Prenatal testing can complicate this as learning that your child is positive for the mutation runs the risk that you’ll also become aware of whether or not you have it. With PGT, it is possible for the embryos to be screened and an unaffected one implanted without the parent learning their own status.
Confirmatory and diagnostic testing
Confirmatory genetic testing, or diagnostic testing, is intended to establish a clinical Huntington’s diagnosis for someone who is already experiencing symptoms, whether or not they’re aware of a family history of the disease.
A doctor might refer you for genetic testing if you come to the clinic with signs and symptoms indicative of Huntington’s. This also includes children with signs of juvenile Huntington’s disease.
If results are positive, it can confirm the diagnosis and enable treatment to start. If it is negative despite the presence of symptoms consistent with Huntington’s, doctors may need to reevaluate the diagnosis in the patient and possibly any affected family members.
Presymptomatic or predictive testing
People with a family history of Huntington’s may choose to be tested for the disease-causing mutation at an early age before symptoms appear, which is called presymptomatic or predictive testing. This may help predict whether they’ll develop symptoms of Huntington’s at some point in their lives.
The Huntington’s Disease Society of America (HDSA) and the National Society of Genetic Counselors currently do not support predictive genetic testing in anyone younger than 18 years old.
The reasoning, which experts generally agree with, is that currently there isn’t any known medical benefit to performing a presymptomatic test this early, but there are significant drawbacks to doing so. Children may not be able to fully understand the implications of genetic testing or may be vulnerable to pressure from others, and the likelihood of experiencing significant psychosocial harm is high.
Benefits and limitations of genetic testing
For some, having the knowledge of whether or not they have or will develop Huntington’s eliminates uncertainty and gives them the chance to better plan for their life in the future.
Benefits of genetic testing for Huntington’s may include:
- making family planning choices, including whether or not to have biological children, terminate a pregnancy, or opt for IVF with preimplantation testing
- planning for a future with or without Huntington’s, including decisions about finances, career, or retirement
- feeling a sense of relief, should results be negative
- having the option to participate in clinical trials or research studies about Huntington’s disease, if results are positive.
Still, there are potential drawbacks to choosing genetic testing, including:
- psychological distress from a positive test result, including depression, anxiety, or worry about when symptoms will start or the course the disease will take
- the fact the test result cannot change what will happen — as there is currently no cure or treatments that can slow or prevent the disease — potentially leading to unnecessary emotional stress
- the possibility that test results will be inconclusive, leading to emotional distress
- survivor’s guilt if the test is negative but other family members carry Huntington’s-causing mutations
- potential workplace discrimination and other barriers including difficulties obtaining life insurance, disability insurance, or long-term care insurance after a diagnosis.
Genetic counseling
The decision to be tested for Huntington’s disease — and when to be tested — is extremely personal and is likely to be a difficult decision. There’s a lot to consider, including how a positive test result will impact you and your loved ones emotionally, financially, or otherwise.
Genetic counselors are trained professionals who can make sure everyone involved understands Huntington’s disease and genetic testing and help them make informed decisions about whether or not to be tested.
Before having genetic testing, genetic counselors will talk you through Huntington’s disease inheritance and all of the possible benefits and limitations of testing.
Their main focus will be on the possible emotional impacts of receiving genetic testing results — whether positive, negative, or indeterminate — and how that may affect your close relationships and life going forward. Genetic counseling for Huntington’s disease is also an opportunity to discuss other factors related to genetic testing, such as insurance and finances.
Genetic counselors are trained to be nonjudgmental and nondirective — they are not trying to tell you what choice to make. Rather, their goal is to make sure that you have all the information you need to make a decision that feels right for you.
After undergoing a genetic test, you’ll likely meet with a genetic counselor again to discuss the results and what they mean.
Where to get genetic testing for Huntington’s disease
Genetic testing for Huntington’s disease is usually done at specialized centers with expertise in testing for Huntington’s disease and all the considerations that come with it. In the case of prenatal and preimplantation genetic testing, the procedure may be done at a specialized fertility clinic with expertise in reproductive genetics.
If you’re looking to start the process of any type of testing for Huntington’s, it’s a good idea to discuss it with your primary care doctor. They can talk you through your options and refer you to a specialized genetic testing center.
The HDSA provides an online tool for locating centers in the U.S. that follow its genetic testing guidelines, which can help you find where to get genetic testing for Huntington’s disease in your area.
The DNA test for confirmatory and predictive testing is a relatively straightforward laboratory procedure. Though the testing process should involve multiple sessions with healthcare professionals before the actual test, including:
- a neurologist who’ll examine you and look for any subtle Huntington’s symptoms
- a psychologist who will assess your current mental health status and make sure you’re emotionally stable prior to testing
- a genetic counselor to talk through the decision for genetic testing.
Once those steps are completed, a blood sample is drawn at the testing center. The sample will be sent to a lab for analysis, and the results might take several weeks to be ready. Usually there’s a follow-up appointment with a genetic counselor to discuss the results in person once they’re available.
The cost of genetic testing for Huntington’s disease may vary based on a number of different factors, but it is usually about $1,000. Health insurance companies may cover testing if it’s recommended by a doctor.
Huntington’s Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- The invisible battle of staying present with Huntington’s disease
- Combining 2 drugs could slow nerve cell death in Huntington’s: Study
- Your voice matters to the Huntington’s disease community
- Tiny systems that keep my life moving with Huntington’s disease
- UK company selects HRN001 as its lead Huntington’s therapy candidate
Related articles
-
 Discussion
Discussion
-
-
-