
Xenazine (tetrabenazine) for Huntington’s disease
Last updated May 30, 2024, by Marisa Wexler, MS

What is Xenazine for Huntington’s disease?
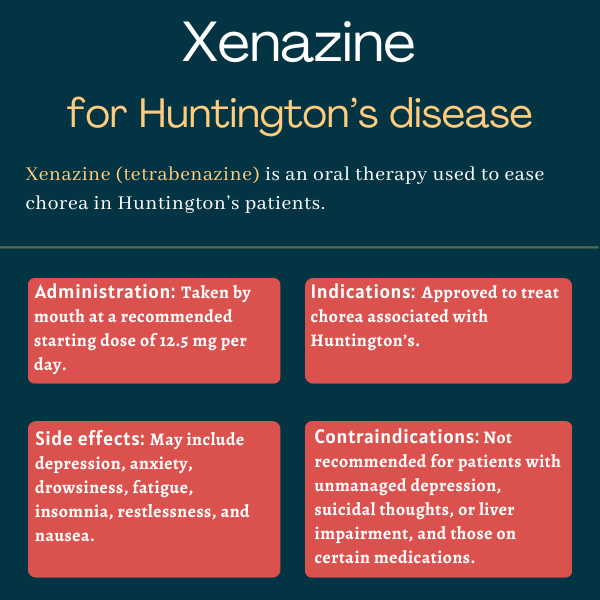
Xenazine (tetrabenazine) is an oral therapy approved to ease chorea, the irregular and uncontrolled movements that affect most people with Huntington’s disease.
Xenazine is sold in the U.S. by Lundbeck Pharmaceuticals. It is marketed by other companies under the brand name Nitoman in Canada and certain European countries, including Germany. Generic versions are available as well.
The therapy is also approved for other movement disorders, including tardive dyskinesia, in certain countries such as the U.K., but not the U.S.
Therapy snapshot
| Brand name: | Xenazine |
| Chemical name: | Tetrabenazine |
| Usage: | Used to treat chorea associated with Huntington’s |
| Administration: | Oral tablets |
How does Xenazine work?
Huntington’s, a neurodegenerative disease caused by genetic mutations, is marked by motor and nonmotor symptoms. Chorea, or involuntary jerking and writhing movements that can involve several parts of the body, is estimated to affect about 90% of Huntington’s patients.
These abnormal movements are thought to be caused by increased levels of dopamine, a major brain chemical messenger, or neurotransmitter, that is involved in movement control.
The exact mechanisms behind Xenazine’s anti-chorea effects aren’t fully understood, but they are thought to be associated with the small molecule’s ability to reduce dopamine signaling in the brain.
Xenazine does this through two different mechanisms. The first is by blocking the vesicular monoamine transporter 2 (VMAT2), a protein responsible for putting dopamine and other neurotransmitters inside tiny vesicles in nerve cells.
Neurotransmitters remain stored in vesicles until the moment the nerve cell fires. At this point, the chemical messengers are released into the synapse, the point of near contact between nerve cells, where they can communicate with each other.
By strongly binding to, and blocking, VMAT2, Xenazine prevents the storage of dopamine and other neurotransmitters in vesicles and their subsequent release into synapses. As a result, dopamine signaling is impaired.
Based on lab results, Xenazine is also thought to reduce dopamine signaling by weakly blocking dopamine receptors at the surface of neurons at the synapse. By doing so, the therapy is thought to prevent dopamine from passing the signal to neighboring neurons, reducing their activation.
These effects on dopamine levels and signaling are expected to help ease chorea in people with Huntington’s.
Who can take Xenazine?
Xenazine was approved by the U.S. Food and Drug Administration (FDA) in August 2008 to treat chorea associated with Huntington’s. This decision made Xenazine the first FDA-approved medication for any Huntington’s symptom.
It’s also approved for this indication in Canada and Europe.
Who should not take Xenazine?
Xenazine’s prescribing information carries a boxed warning noting it may increase the risk of depression and suicidal thoughts or behaviors (suicidality) in people with Huntington’s. As such, the therapy is not recommended for anyone with untreated or inadequately treated depression or who is suicidal.
Xenazine is also contraindicated in patients with liver problems, as the therapy is mostly metabolized by that organ.
The therapy is not recommended for people on certain other medications. These include:
- Reserpine, an old medication for high blood pressure and to treat Huntington’s abnormal movements. Those switching from reserpine to Xenazine should wait 20 or more days after the last reserpine dose before making the switch.
- Monoamine oxidase inhibitors (MAOIs), a type of antidepressant. Xenazine should not be taken in the first two weeks after MAOI treatment discontinuation.
- Medications known to cause QT prolongation — which is an extension of the interval between the heart contracting and relaxing — including certain antipsychotics and antibiotics.
- Other approved treatments for Huntington’s-associated chorea, such as Austedo or Austedo XR (deutetrabenazine) and Ingrezza or Ingrezza Sprinkle (valbenazine).
Xenazine also should be avoided in patients with QT prolongation and a history of arrhythmias, or abnormal heartbeat.
How is Xenazine administered in Huntington’s disease?
Xenazine is available as tablets taken by mouth with or without food. Tablets come in two dosage strengths:
- 12.5 mg white, cylindrical tablets, nonscored and carved with “CL” and “12.5” on one side
- 25 mg yellowish, cylindrical tablets, scored and carved with “CL” and “25” on one side.
Dosage is determined on an individual basis based on how each patient responds to the therapy. The recommended starting dose is one 12.5 mg tablet, taken in the morning. After the first week of treatment, patients should increase their daily dose to 25 mg, taken as one 12.5 mg tablet twice a day.
The daily dose can then be slowly increased each week, by 12.5 mg, to find the optimal dose for each patient. If a dose of 37.5 or 50 mg per day is needed, a three-times-per-day dosing schedule should be used. A single dose of Xenazine should not exceed 25 mg.
If daily doses higher than 50 mg are needed, patients should first be tested for activity of CYP2D6, the liver enzyme mainly responsible for breaking down Xenazine. In patients who have intermediate or high CYP2D6 activity, the dose can continue to be increased by 12.5 mg/day each week, up to a maximum daily dose of 100 mg, taken on a three-times-per-day dosing schedule and with each single dose not exceeding 37.5 mg.
In patients with low CYP2D6 activity or those taking other medications that are strong CYP2D6 suppressors — including certain antidepressants — the daily dose should not exceed 50 mg and each single dose should not exceed 25 mg.
If patients develop side effects such as mental health problems or movement disorders during the dosage-finding period, the dose of Xenazine should be reduced. If this does not resolve the side effects, patients may need to discontinue Xenazine or receive other supportive treatments.
If Xenazine treatment is paused for five days or less, treatment can be resumed at the prior maintenance dose. However, if treatment is paused for more than five days, patients should restart the process of dose optimization, starting at a dose of 12.5 mg per day.
The therapy can be discontinued without tapering the dose. Once it is discontinued, chorea may reemerge within 12 to 18 hours of the last dose.
Xenazine in clinical trials
Xenazine’s approval for Huntington’s-associated chorea in the U.S. was based mainly on the results of the Phase 3 TETRA-HD clinical trial (NCT00219804), conducted by the Huntington Study Group.
TETRA-HD
The TETRA-HD study was a multicenter, placebo-controlled study of 84 patients with Huntington’s who could still walk. Participants were randomly assigned to receive either Xenazine or a placebo for 12 weeks, or about three months. Fifty-four patients received the therapy, up to a maximum dose of 100 mg/day. Xenazine’s dose optimization took place in the first seven weeks of treatment, after which a stable maintenance dose was administered.
The study’s main goal was to determine the effect of treatment on the Total Maximal Chorea (TMC) score of the Unified Huntington’s Disease Rating Scale (UHDRS). This scale measures chorea on a scale from 0 to 4 across seven parts of the body, for a total possible score of 0 to 28. Higher scores reflect more severe chorea.
Results showed Xenazine decreased chorea severity by a mean of 5 points on the UHDRS’ TMC score, whereas the placebo led to a 1.5-point drop on average — a statistically significant difference.
Compared with those on the placebo, a significantly greater proportion of Xenazine-treated patients experienced a chorea score reduction of at least 3 points (69% vs. 23%), 6 points (50% vs. 7%), and 10 points (19% vs. 3%).
Within a week after stopping treatment, average chorea scores worsened more in the Xenazine group than in the placebo group.
In addition, patients on Xenazine were significantly more likely to experience at least minimal global improvement — as assessed by clinicians with the Clinical Global Impression-Global Improvement Scale — than those given a placebo (69% vs. 24%).
Other measures of functionality and cognition were generally comparable between the groups, though a clinician-rated measure of ability to perform certain tasks of daily living worsened by significantly more in the Xenazine group.
Extension study
Participants who completed the placebo-controlled portion of TETRA-HD had the option to enroll in an extension study in which all were treated with Xenazine for up to 80 weeks (about 1.5 years). Of the 75 patients who entered the extension study, 45 remained for the full 80 weeks.
Results showed a significant 4.6-point reduction on the UHDRS’ TMC score, indicating sustained benefits with longer-term treatment. One week after Xenazine discontinuation, chorea reemerged with an average score increase of 5.3 points.
Withdrawal study
A separate five-day study included 30 people with Huntington’s who had been on Xenazine for at least two months. A total of 12 patients were switched to a placebo after one day, and another 12 were switched to a placebo after three days. The remaining six patients remained on Xenazine for all five days.
Consistent with findings from TETRA-HD, results showed that withdrawing Xenazine on day one led to a greater increase in TMC score on the UHDRS relative to those who were switched to a placebo after three days and those who remained on Xenazine.
Common side effects of Xenazine
The most common side effects of Xenazine include:
- sleepiness or sedation
- fatigue
- insomnia
- depression
- akathisia, a movement disorder that makes it difficult for a person to remain still due to an inner restlessness
- anxiety or worsened anxiety
- nausea.
Depression and suicidality
Xenazine’s label carries a boxed warning noting it may increase the risk of depression and suicidality in Huntington’s patients, who are already at a higher risk for these issues. In clinical trials of the therapy, up to about one-third of patients on Xenazine experienced depression or worsening depression.
The need for Xenazine should be carefully weighed against these risks when deciding whether or not to start the medication. Patients taking Xenazine, as well as their caregivers and families, should be instructed to look for signs of worsening mental health and concerning behaviors. The presence of such signs should be reported to a healthcare professional immediately. If depression or suicidality while on Xenazine does not resolve or cannot be managed, treatment discontinuation should be considered.
Clinical worsening versus side effects
In a clinical trial lasting about three months, Xenazine was associated with a slight worsening of mood, cognition, rigidity, and functional capacity — issues that are already associated with Huntington’s. It’s not known if these effects persist with longer-term treatment.
The need for Xenazine should be periodically reviewed, assessing both its effect on chorea and any unwanted effects. It may be difficult to tease out Xenazine’s side effects from Huntington’s progression without pausing treatment or reducing the dosage.
Neuroleptic malignant syndrome
There have been reports of a potentially fatal complication called neuroleptic malignant syndrome (NMS) in people treated with Xenazine and other dopamine signaling-reducing drugs.
NMS symptoms include high fever, muscle rigidity, altered mental status, and changes in heart rhythm and blood pressure. If such signs and symptoms are detected, Xenazine should be immediately discontinued, and appropriate treatment and monitoring should be undertaken.
If Xenazine is needed in patients who have previously experienced NMS while on the therapy, monitoring for signs of NMS recurrence is required.
Movement disorders
Xenazine may cause restlessness, agitation, akathisia, and parkinsonism, a movement disorder marked by motor symptoms similar to those seen in Parkinson’s disease, such as slowed movement, rigidity, and tremor.
Patients on Xenazine should be monitored for these side effects. If akathisia or parkinsonism develop, the treatment dose may need to be reduced or the medication discontinued.
The risk of these movement disorders may be increased in Xenazine-treated patients also taking antipsychotics or medications that suppress dopamine.
Sedation and sleepiness
Sedation or sleepiness is the most common dose-limiting side effect of Xenazine. In clinical trials, reducing the dosage helped ease sedation for most patients, but this side effect can also occur with lower-than-recommended dosages.
Patients starting on the medication should not drive, operate dangerous machinery, or undertake other actions that require alertness until they know how the medication affects them.
Drinking alcohol or taking sedating medications may worsen sedation and sleepiness while on Xenazine.
Irregular heartbeat
Xenazine can cause a type of irregular heartbeat known as QTc prolongation. The medication should not be used in patients with a syndrome associated with QT prolongation or with a history of arrhythmias.
In addition to these clinical features, having deficient levels of potassium or magnesium and using other medications that cause QT prolongation can increase the risk of serious heart events in people on therapies that increase QT prolongation.
Orthostatic hypotension
Xenazine may cause orthostatic hypotension, where blood pressure drops suddenly when a person rises or stands, resulting in feelings of lightheadedness, dizziness, or, in extreme cases, fainting. Patients vulnerable to low blood pressure should be considered for monitoring of vital signs upon standing.
Increased prolactin levels
Xenazine can increase blood levels of prolactin, a hormone that helps to regulate lactation and breast development. High prolactin levels can result in abnormal breast tissue growth, impotence, changes in menstruation, and bone health problems. Some data suggest it may increase the growth of certain breast cancers, so caution is advised when considering Xenazine in patients with a history of breast cancer.
However, the clinical significance of increased prolactin is unclear for most people. If patients experience symptoms that may be caused by excessive prolactin levels, they should undergo appropriate testing and consider discontinuing treatment.
Binding to melanin-containing tissues
The active agent in Xenazine and its byproducts bind to melanin, which is the brownish pigment that gives skin its shade and helps determine eye color. The clinical significance of these effects is unclear, but there’s theoretically a risk that the therapy may build up to toxic levels in these tissues over time. Therefore, clinicians prescribing Xenazine should be aware of the possibility of eye complications in patients on the therapy.
Use in pregnancy and breastfeeding
No adequate data are available on the use of Xenazine in people who are pregnant or breastfeeding. In animal studies, administering Xenazine during pregnancy and lactation resulted in an increased risk of death for the offspring.
It also is not known if Xenazine can be found in human breast milk and whether it has any impact on nursing infants or on milk production.
Patients who are pregnant or breastfeeding or who plan to become pregnant or breastfeed should consult with their healthcare providers, carefully weighing the potential risks and benefits of treatment.
Huntington’s Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Ingrezza engages with therapeutic target more strongly than Austedo
- Anticipation of a possible new clinical trial has us holding on to hope
- What caregiver burnout is really about — and what you can do about it
- Oral Huntington’s treatment aims to slow disease progression
- Accepting help from my loved one with HD is a lesson in partnership
- Understanding how Huntington’s disease affects my cognition
- Guest Voice: We hold onto hope while fighting for new treatments
- Top 5 Huntington’s disease news stories of 2025
- Another year means treasuring more moments of shared joy
- Faulty cellular waste disposal system may drive Huntington’s: Study


