CHCHD2 protein loss in brain may drive disease long before onset
Brain organoid study finds HTT mutations affect mitochondria
Written by |
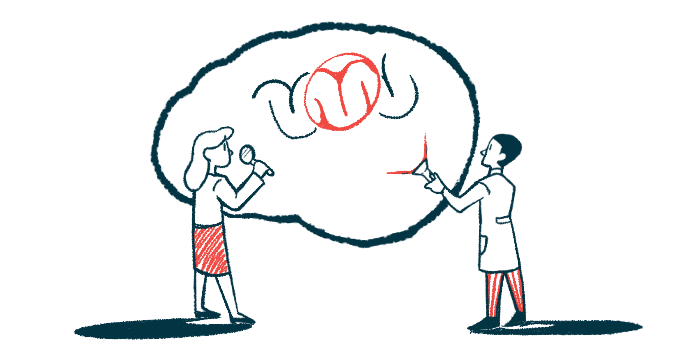
Diminished production in the brain of a protein known as CHCHD2 may contribute to early neurodevelopmental changes that go on to drive Huntington’s disease, a study reports, with scientists poising the gene responsible for its production as a possible therapeutic target.
CHCHD2 is involved in maintaining the workings of mitochondria, the organelles inside cells that are responsible for generating energy. The protein’s loss has been implicated in Parkinson’s disease, but never before in Huntington’s.
Scientists in Germany, working with brain-like organoids (three-dimensional structures resembling human brains at early stages) found that HTT gene mutations — the disease’s cause — resulted in low CHCHD2 levels and metabolic disturbances early in the organoids’ development. Increasing CHCHD2 production helped to restore mitochondrial health and cellular energy.
“We were surprised to find that Huntington’s disease can impair early brain development through defects associated with mitochondrial dysfunction,” Pawel Lisowski, PhD, a study co-first author at the Max Delbrück Center for Molecular Medicine, in Berlin, said in a institute press release.
“The organoid model suggests that HTT mutations damage brain development even before clinical symptoms appear, highlighting the importance of detecting the late-onset neurodegenerative disease early” said Selene Lickfett, the study’s other co-first author and a doctoral student at Heinrich Heine University Düsseldorf.
The study, “Mutant huntingtin impairs neurodevelopment in human brain organoids through CHCHD2-mediated neurometabolic failure,” was published in Nature Communications.
Organoids can mimic brain cell interactions, properties better than animal models
Mutations in the HTT gene lead to the production of a mutant huntingtin protein (mHTT) that toxically accumulates in nerve cells. Over time, the resulting damage to nerve cells is deadly.
The mechanisms linking mutant huntingtin to neurodegeneration are not fully known. Emerging evidence indicates that it might disrupt brain development early in a person’s life, perhaps before nerve cells are fully mature, the scientists noted.
“In mice, targeted HTT [protein] disruption is embryonic lethal, brain-specific HTT inactivation leads to progressive neuronal defects, and extensive HTT reduction fails to support normal brain development,” they wrote.
To better determine how mHTT influences early brain development, the scientists used human stem cells to generate brain organoids, mini-brains that can more fully mimic the properties and cellular interactions of the human brain than animal models.
Some of the organoids were grown from stem cells engineered to house Huntington’s-causing mutations. These mutant mini-brains showed significant impairments in normal neurodevelopment and changes in gene activity related to nervous system development. In particular, neural progenitors that give rise to mature nerve cells seemed to be disrupted.
Gene activity in the organoids revealed that the CHCHD2 gene, which provides instructions to produce a protein of the same name, had lower than normal activity across all stages of neurodevelopment.
Findings were similar at the protein level, with mutant organoids showing reduced CHCHD2 protein levels relative to organoids without mutations.
Mutant HTT seen to affect CHCHD2, impact mitochondria in early nerve cells
Mutated mini-brains also showed disrupted metabolic processes in nerve cells and widespread mitochondrial dysfunction, particularly in neural progenitors.
“These findings suggest that mHTT leads to CHCHD2 dysregulation, which in turn impairs mitochondrial function and organization in early neural cells,” the researchers wrote.
Lab-grown neural progenitors derived from Huntington’s patients showed problems in neurodevelopment and mitochondrial regulation similar to the brain-like organoids.
Notably, these defects were evident before the accumulation of toxic clumps of mutated huntingtin protein, suggesting that detrimental changes could happen in the Huntington’s brain well before the disease’s clinical onset.
“The prevalent view is that the disease progresses as a degeneration of mature neurons,” said Alessandro Prigione, MD, PhD, the study’s senior author and a professor of pediatric metabolic medicine at the Düsseldorf university. “But if changes in the brain already develop early in life, then therapeutic strategies may have to focus on much earlier time-points.”
Possible need for intervention long before disease onset in adults
Adult interventions might not be effective, the researchers noted. Should therapeutic strategies be “given during adult life, the brain [circuitry] has already been altered and may not be effectively repaired anymore,” they wrote.
Other organoids were grown without Huntington’s-associated mutations in the HTT gene through gene-editing strategies, restoring normal CHCHD2 levels and reversing energy defects.
A similar gene therapy approach, Prigione suggested, may be of benefit for treating Huntington’s disease.
Restoring CHCHD2 gene activity in lab-grown human nerve cells with a Huntington’s-causing mutation also reversed the mitochondrial abnormalities observed in the mutant mini-brains.
“That was surprising,” Lickfett said. “It suggests in principle that this gene could be a target for future therapies.”
CHCHD2, the scientists concluded, “could represent a target for early intervention … as its modulation would impact mitochondrial morpho-function [relationship between a system’s form and function], which in turn could be important for … neurodevelopment on the one hand and for overall systemic metabolic resilience on the other.”