Discussion
Discussion
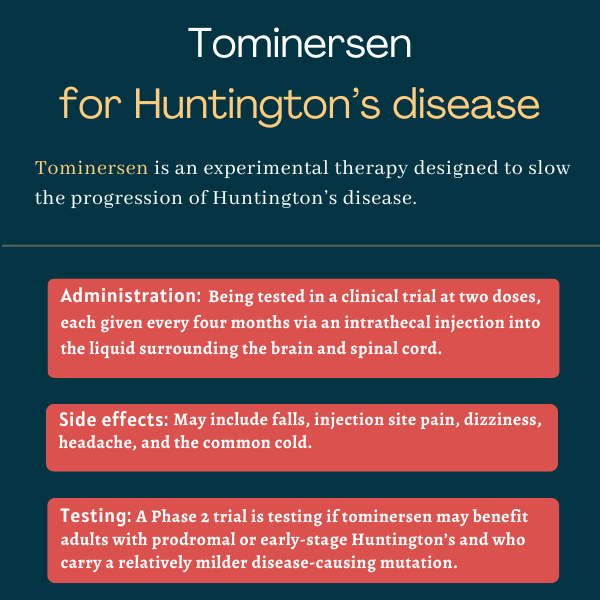
Tominersen for Huntington’s disease
Last updated June 6, 2024, by Marisa Wexler, MS

What is tominersen for Huntington’s disease?
Tominersen, previously IONIS-HTTRx and RG6042, is an experimental injectable treatment being developed by Roche to slow or prevent the progression of Huntington’s disease.
It was the first treatment in clinical development that sought to target Huntington’s underlying cause by reducing the production of the abnormal protein that drives the disease.
The therapy was originally discovered by Ionis Pharmaceuticals and initially developed for Huntington’s in collaboration with Roche, which acquired its worldwide development and commercialization rights in late 2017.
Roche stopped dosing in most clinical trials testing tominersen in Huntington’s patients in 2021 after interim data from a Phase 3 trial indicated the therapy was not benefiting participants.
The company is now running a new Phase 2 trial to test tominersen in people with prodromal Huntington’s or at an early stage of the disease. The prodromal period is characterized by the presence of early signs and nonspecific symptoms of Huntington’s.
Tominersen received orphan drug status for treating Huntington’s in the U.S. and Europe, and won priority medicine (PRIME) designation for the same indication in Europe. Both designations are meant to expedite its clinical development and regulatory review by providing a range of financial incentives and support.
Therapy snapshot
| Treatment name: | Tominersen |
| Administration: | An injection into the spinal canal |
| Clinical testing: | Previously tested in a Phase 3 trial that was stopped early due to negative interim results; now being tested in a different patient subpopulation within a Phase 2 trial |
How does tominersen work in Huntington’s disease?
Huntington’s is a neurodegenerative disorder caused by excessive repeats of three DNA building blocks — CAG — in the HTT gene. This leads to an abnormal, or mutant, huntingtin protein being produced that forms toxic clumps inside nerve cells.
This is thought to drive the neurodegeneration that marks the disease in several brain regions and that causes symptoms, including motor problems, cognitive impairment, and behavioral and psychiatric problems.
Tominersen is an antisense oligonucleotide (ASO), or a short piece of genetic material, that’s designed to bind to the HTT gene’s messenger RNA (mRNA), an intermediary molecule derived from DNA that guides protein production.
By doing so, the therapy marks HTT mRNA molecules for destruction, preventing huntingtin protein, including its mutant version, from being produced.
But as ASOs cannot naturally enter the brain and spinal cord, which are the target tissues of therapies for neurological diseases such as Huntington’s, tominersen is administered directly into the liquid that bathes these tissues, called the cerebrospinal fluid (CSF).
This way, it should reduce the formation of toxic huntingtin clumps in the brain, slowing or preventing Huntington’s progression.
How will tominersen be administered in Huntington’s disease?
Tominersen is administered via an injection into the spinal canal that delivers the medication directly to the CSF. This type of injection is called an intrathecal injection.
In previous Huntington’s trials, the therapy was tested at a dose of up to 120 mg, given once monthly, once every other month, and once every four months. In the ongoing Phase 2 clinical trial, tominersen is being tested at lower doses, 60 mg and 100 mg, given once every 16 weeks.
Tominersen in Huntington’s disease clinical trials
Treatment with ASOs similar to tominersen was shown to suppress huntingtin production, delay disease progression, and reverse some motor and behavioral deficits in mouse models of Huntington’s. This led Ionis to begin testing tominersen in Huntington’s clinical trials.
Early studies
Ionis launched a Phase 1/2a trial (NCT02519036) in 2015 to evaluate tominersen’s safety, tolerability, and pharmacological properties against a placebo in adults, ages 25-65, with early-stage, or early manifest, Huntington’s.
Forty-six patients were randomly assigned to receive four monthly intrathecal injections with either one of five doses of tominersen (10, 30, 60, 90, or 120 mg; 34 patients) or a placebo (12 patients).
Results indicated tominersen safely decreased CSF levels of mutant huntingtin — by 38% with the 120 mg dose — while patients on a placebo saw their levels increase by 10%.
All the patients who completed the trial chose to enroll in an open-label extension study (NCT03342053), where they received tominersen injections at 120 mg once a month or once every two months for 15 months, or little over a year.
The less frequent dosing regimen was enough for patients to reach target reductions in CSF levels of mutant huntingtin. This, along with similar pharmacological properties and a more favorable safety and tolerability profiles relative to the once-monthly dosing regimen, supported further testing of less frequent dosing regimens.
GENERATION HD1
To further evaluate the safety and efficacy of tominersen’s less frequent dosing regimens in a larger number of patients, Roche launched in early 2019 a Phase 3 trial called GENERATION HD1 (NCT03761849). A total of 791 adults with established, or manifest, Huntington’s, were recruited at about 100 sites around the world.
Participants were randomly assigned to one of three groups. The first group received tominersen once every two months, the second group was given tominersen once every four months, receiving a placebo at alternate weeks, and the third group took a placebo every other month.
Both tominersen, given at 120 mg, and the placebo were meant to be given via intrathecal injections for up to 101 weeks, or just over two years.
The study’s main goal was to assess changes in disease severity, as assessed with the composite Unified Huntington’s Disease Rating Scale (cUHDRS) that accounts for cognition, motor skills, and the ability to function independently in daily life (total functional capacity, or TFC). Outside the U.S. and Japan, changes in TFC scores were designated as the main outcome. In both measures, lower scores indicate worse disability.
Roche announced in March 2021 that tominersen dosing in GENERATION HD1 would stop. The decision was made after a pre-planned assessment of data from an independent panel of experts demonstrated the therapy wasn’t showing a favorable benefits/risk profile.
Specifically, results after little more than a year showed those given tominersen once every four months had similar mean changes on cUHDRS and TFC scores relative to those on a placebo.
Those receiving tominersen every other month had a significantly greater drop in cUHDRS scores than the other two groups. The more-frequent dosing also was associated with a higher rate of serious adverse events.
Dosing in GEN-EXTEND (NCT03842969), an open-label extension Phase 3 study evaluating tominersen’s long-term safety and tolerability in people who participated in other tominersen trials, also was paused after GENERATION HD1’s interim analysis.
After GENERATION HD1 ended, researchers conducted post hoc analyses to look for subgroups of patients who might have shown any signs of benefit from tominersen. Post hoc analyses are investigations designed and carried out after all trial data have been collected.
In these analyses, participants were divided into four subgroups based on age and CAP score: low age/low CAP, high age/high CAP, low age/high CAP, and high age/low CAP.
The CAP score is a measure of disease severity that looks at age along with the number of CAG repeats in the HTT gene, with a higher repeat number being indicative of a more severe Huntington’s-causing mutation. The patients’ median age was 48, and the median CAP score was 500.
The researchers found that, across all four subgroups, those given tominersen every other month had worse cUHDRS and TFC scores than those given a placebo. But among those treated once every four months, the low age/low CAP subgroup tended to have higher cUHDRS and TFC scores relative to those on a placebo.
Ongoing GENERATION HD2
Based on the potentially positive signs of tominersen, given every four months, in this subgroup of younger patients with less severe disease-causing mutations, Roche launched the global Phase 2 GENERATION HD2 trial (NCT05686551) in 2023 to test this hypothesis.
The ongoing study seeks to enroll up to 300 adults, ages 25-50, with a CAP score between 400 and 500 and who have prodromal or early-stage Huntington’s. Eligible participants must never have used an ASO therapy or other mutant huntingtin-lowering treatment.
Participants are randomly assigned to receive intrathecal injections of either one of two doses of tominersen (60 or 100 mg) or a placebo, once every four months for at least 16 months.
GENERATION HD2’s main goals include examining the therapy’s safety and its effects on CSF levels of mutant huntingtin, as well as on cUHDRS and TFC scores. Secondary goals include changes in several measures of cognitive and motor function, and CSF levels of a nerve damage biomarker called neurofilament light chain. Researchers will also monitor for antibodies against the therapy.
After completing the study’s placebo-controlled period, participants may have the option to enroll in its open-label extension phase, where all will be given tominersen for a longer period.
The GENERATION HD2 study is expected to end in 2027.
Common side effects of tominersen
In clinical testing so far, tominersen has been found to be generally safe and well tolerated, with generally similar rates of adverse events relative to a placebo. The most commonly reported adverse events in the Phase 3 GENERATION HD1 trial included falls, headaches, dizziness, common cold, and complications associated with the intrathecal injections used to administer the therapy.
Huntington’s Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- I insist on being seen as I am, not as someone else’s story
- FDA requests additional clinical trial of Huntington’s gene therapy AMT-130
- A log cabin miles from anywhere was just what the doctor ordered
- The invisible battle of staying present with Huntington’s disease
- Combining 2 drugs could slow nerve cell death in Huntington’s: Study
Related articles
-
 Discussion
Discussion
-
-
-