AMT-130 for Huntington’s disease
Last updated Dec. 17, 2024, by Marisa Wexler, MS

What is AMT-130 for Huntington’s disease?
AMT-130 is an experimental gene therapy being developed by uniQure to slow the progression of Huntington’s disease.
The medication received orphan drug designation for the treatment of Huntington’s in the U.S. in 2017 and in Europe the following year. In the U.S., it also was given fast track status in 2019 and a regenerative medicine advanced therapy (RMAT) designation in 2024 for the same indication. All of these designations are meant to expedite the therapy’s clinical development and regulatory review by providing a range of financial incentives and regulatory support.
Therapy snapshot
| Treatment name: | AMT-130 |
| Administration: | Being tested in Huntington’s as a one-time infusion, given directly into the brain via a surgical procedure |
| Clinical testing: | Currently in Phase 1/2 clinical trials |
How does AMT-130 work in Huntington’s disease?
Huntington’s is caused by mutations in the huntingtin (HTT) gene, which provides instructions for making the huntingtin protein. This gene contains CAG repeats, a series of three DNA building blocks that are repeated 10 to 35 times in a row. But in Huntington’s, these CAG repeats are present at excessive numbers, often 40 or more.
The result is an abnormal version of the huntingtin protein that is longer than usual and prone to forming toxic clumps in nerve cells, causing a range of motor and nonmotor disease symptoms.
AMT-130 is designed to reduce the production of both normal and mutated huntingtin protein by targeting the HTT gene’s messenger RNA (mRNA), which is an intermediary molecule derived from DNA that guides protein production.
The gene therapy uses a modified and noninfectious viral vector called adeno-associated virus serotype 5 (AAV5) to deliver to cells a human-made piece of genetic material known as microRNA. The microRNA is designed to bind to HTT mRNA molecules and prevent their use to produce huntingtin.
To target mostly brain nerve cells, AMT-130 is administered directly into the caudate nucleus and the putamen, two deep brain regions that are heavily impacted by Huntington’s.
By lowering production of the toxic huntingtin protein in the brain, the one-time gene therapy is expected to ease symptoms and slow or stop disease progression in people with Huntington’s disease.
How will AMT-130 be administered in Huntington’s disease?
In Huntington’s clinical trials, AMT-130 has been tested at a low dose (6 trillion vector genomes, or virus units) and a high dose (60 trillion vector genomes). The therapy was administered directly into the caudate nucleus and putamen via a surgical procedure.
The procedure involved inserting a very small catheter (tube) to deliver the gene therapy into three different parts of these deep structures, and on each side of the brain. The infusions are given over a period of eight to 10 hours, and clinicians use magnetic resonance imaging (MRI) to track the therapy’s delivery.
Research suggests that, after administration, the gene therapy spreads throughout the caudate nucleus and putamen before moving outward to other parts of the brain.
AMT-130 in Huntington’s disease clinical trials
The safety, tolerability, and efficacy of AMT-130 are being evaluated in two ongoing Phase 1/2 clinical trials: a placebo-controlled study taking place in the U.S. (NCT04120493) and an open-label trial in Europe (NCT05243017).
Both trials are designed to test the therapy in adults, ages 25-65, with early Huntington’s — up to 37 adults in the U.S. trial and 14 in the European study. All treated patients are expected to receive a single administration of AMT-130, after which they will be followed up for up to five years.
In both studies, a first group of participants is given a low dose of AMT-130 (6 trillion vector genomes) and a second group is given a higher dose (60 trillion vector genomes).
But in the U.S. study, patients recruited for the first two groups are randomly assigned to either an AMT-130 infusion or an imitation (sham) surgical procedure. After one year, these patients will know what they received, and those given the sham procedure have the option of receiving the gene therapy. They will be followed until the study’s end.
For both trials, the main goal is to assess the therapy’s safety and tolerability, while the secondary goal is to evaluate how long AMT-130 stays in the brain.
Changes in measures of disease severity, functional capacity, motor skills, brain parameters, and quality of life also will be evaluated. Researchers also will measure changes in the levels of mutant huntingtin and a nerve damage marker called neurofilament light chain (NfL).
The U.S. trial has completed enrollment of 10 patients in the first group, and 16 adults in the second group. The European study, as of July 2024, has enrolled six participants in its low-dose group and seven in the high-dose group.
One-year interim data showed that AMT-130 given at low-dose halved the levels of mutated huntingtin in the cerebrospinal fluid, the liquid that flows around the brain and spinal cord.
Additional findings from all 39 enrolled patients were announced in late 2023. In the low-dose group, with about 2.5 years of follow-up, patients’ motor function and ability to perform daily activities at last follow-up were comparable with pretreatment measures, implying relatively stable disease. In the high-dose group, neurological function measures showed stability or improvement over about 1.5 years of follow-up.
An additional analysis compared data between 21 patients treated with AMT-130 and followed for at least two years in either trial, and an external group of 154 untreated Huntington’s patients who participated in natural history studies.
This external control group included patients who would meet eligibility criteria for the AMT-130 Phase 1/2 trials, and who were matched to AMT-130-treated patients in terms of demographic and clinical characteristics at the study’s start.
Two-year results found that the 12 patients given AMT-130’s high dose experienced a mean decline of 0.2 points in the composite Unified Huntington’s Disease Rating Scale (cUHDRS), in which lower scores reflect worsening disability. In turn, the external control group experienced a mean one-point drop.
This represented a significant slowing of disease progression, by a mean of 80%, with AMT-130 at high dose.
Nine included patients treated with the low dose showed a mean 0.7-point reduction in the cUHDRS, reflecting a 30% slowing of disease progression relative to the control group. This group difference, however, was not statistically significant.
The high-dose group showed better scores than the control group across most individual components of cUHDRS, including those assessing motor and cognitive function.
AMT-130-treated patients also experienced a significant reduction, by 11%, in NfL levels in the fluid surrounding the brain and spinal cord after two years, while the natural history group saw their levels increase by 26%.
Based on these findings, the U.S. Food and Drug Administration has agreed that data from these trials, compared with an external control group, may be used to support a future submission for AMT-130’s approval.
In both studies, a third group of patients will be randomly assigned to AMT-130 at either low or high dose, along with an immunosuppression regimen given before and after surgery to see if this approach reduces the risk of adverse events.
Both studies are expected to end in 2029.
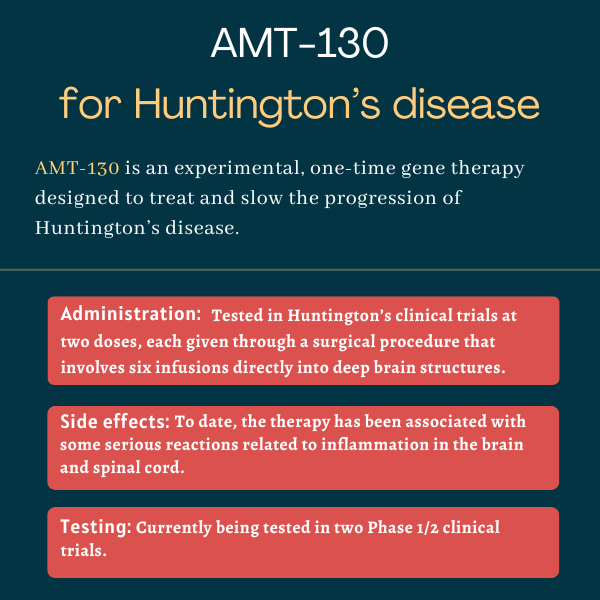
Common side effects of AMT-130
In clinical testing so far, a single administration of AMT-130 has been found to be safe and well tolerated. The most commonly reported adverse events in treated patients are complications related to the surgical procedure that’s used to administer the gene therapy. In some patients, AMT-130 was reported to cause serious side effects associated with inflammation in the central nervous system, the brain and spinal cord.
Huntington’s Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- FDA requests additional clinical trial of Huntington’s gene therapy AMT-130
- A log cabin miles from anywhere was just what the doctor ordered
- The invisible battle of staying present with Huntington’s disease
- Combining 2 drugs could slow nerve cell death in Huntington’s: Study
- Your voice matters to the Huntington’s disease community