New neurons can replace damaged ones in Huntington’s mice
Newly grown nerve cells integrate with brain cells to repair damage
Written by |

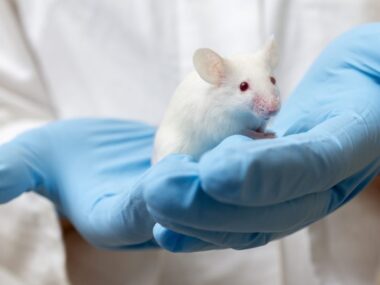
Researchers were able to promote the formation of new neurons that integrated into existing motor circuits and helped repair damage and influence motor behavior in the brain of a mouse model of Huntington’s disease, a study showed.
“Our research shows that we can encourage the brain’s own cells to grow new neurons that join in naturally with the circuits controlling movement,” Abdellatif Benraiss, PhD, senior author of the study and research associate professor at the University of Rochester Medical Center, said in a university news story. “This discovery offers a potential new way to restore brain function and slow the progression of” Huntington’s.”
The study, “Newly generated striatal neurons rescue motor circuitry in a Huntington’s disease mouse model,” was published in Cell Reports.
Huntington’s is a genetic disorder that mainly causes certain brain cells, called medium spiny neurons (MSNs), to sicken and die in a brain region called the striatum. The loss of these nerve cells disrupts normal neuronal signaling, ultimately driving Huntington’s symptoms.
Given that previous research identified certain reservoirs of neural progenitor cells in the brain that are capable of generating new neurons, researchers are actively working to find ways to boost the formation of new MSNs to replace the damaged cells in Huntington’s. Theoretically, this could offer a way to treat the neurodegenerative condition.
BDNF and Noggin at work
Benraiss and colleagues previously showed that increasing levels of two signaling molecules, BDNF and Noggin, in the brain triggered the production of new neurons that matured into MSNs in both mice and non-human primates. In a mouse model of Huntington’s, this approach was associated with slower progression of motor symptoms and longer survival.
However, it wasn’t clear whether these benefits were due to the integration of newly formed MSNs into existing brain circuits and subsequent restoration of damaged circuits, or if other mechanisms might be at work.
To shed light on this issue, the scientists conducted a detailed battery of tests to examine what happens to newly formed MSNs in a mouse model of Huntington’s. Formation of new neurons was triggered by BDNF and Noggin treatment, administered directly into the brain.
“Evidence of circuitry integration is a prerequisite for defining the functional integration of newly introduced neurons,” the researchers wrote.
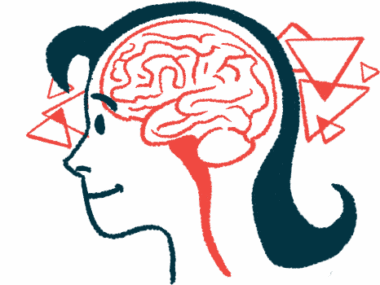
They found that the newly generated cells did sync up with existing neurons, forming new synapses (connections between nerve cells) to create new, working nerve circuits in the brains of adult mice.
“The newly generated MSNs established synaptic connections with … striatal [neurons] in proportions similar to those of already-resident, developmentally generated neurons while extending [nerve fiber] projections to their principal target, the globus pallidus,” the researchers wrote. The globus pallidus is a brain region involved in the regulation of voluntary movement.
Further experiments showed that specifically activating the newly made cells influenced the animals’ motor behavior and significantly increased motor activity.
The results “strongly suggest that new neurons recruited in response to BDNF and Noggin treatment enable the reconstitution of multi-synaptic circuits in the adult brain and, in turn, that these reconstituted striatal circuits account for the slowing in disease progression previously noted in BDNF-Noggin-treated [Huntington’s disease] mice,” the researchers wrote.
“Taken together with the persistence of these progenitor cells in the adult primate brain, these findings suggest the potential for this regenerative approach as a treatment strategy in Huntington’s and other disorders characterized by the loss of neurons in the striatum,” Benraiss said.