Low Oxytocin in CSF Correlates with Social, Cognitive Impairments: Study
Results suggest administering oxytocin could improve social cognition in patients
Reduced levels of oxytocin — a natural hormone produced in the brain’s hypothalamus that also works as a chemical messenger — in the cerebrospinal fluid (CSF) were found in Huntington’s disease patients with cognitive and social impairments, a new study shows.
The findings support oxytocin levels as a biomarker of impaired social skills, as well as administering oxytocin as a potential therapy, according to its researchers.
“Our findings of a relationship between lower oxytocin levels in CSF and reduced social cognition in HD [Huntington’s disease] open up possibilities for treatment trials to evaluate potential effects of administration of oxytocin on social cognition,” the researchers wrote in their study, “Decreased CSF oxytocin relates to measures of social cognitive impairment in Huntington’s disease patients,” which was published in Parkinsonism & Related Disorders.
Huntington’s disease is a genetic neurodegenerative disorder caused by a mutation in the HTT gene. This leads to excessive repeats of a portion of DNA, called CAG triplets, and a longer than normal mutant huntingtin protein being produced.
The mutant huntingtin (mHTT) accumulates to toxic levels inside nerve cells in the brain, causing progressive neurodegeneration.
While the disease is mainly characterized by motor problems, non-motor symptoms can develop, including psychiatric disturbances, which often occur before motor impairments.
Common symptoms include depression, altered social cognition, metabolic changes, sleep disturbances, and altered functioning of the autonomic (involuntary) nervous system.
It’s thought that the psychiatric disturbances in Huntington’s may be linked with alterations in the hypothalamus, a brain region that controls sleep and growth, as well as hormone production.
Analysis of brain tissue from deceased Huntington’s patients has shown alterations to the hypothalamus, including reductions in certain hormone-producing nerve cells.
Link between social cognition, oxytocin explored
In one study, a 45% decrease in the nerve cells producing oxytocin in the brain of people with Huntington’s disease was reported compared to those without the disease. In another study, this reduction in oxytocin-expressing neurons in the hypothalamus was seen without changes in the striatum, a brain region involved in voluntary movement control.
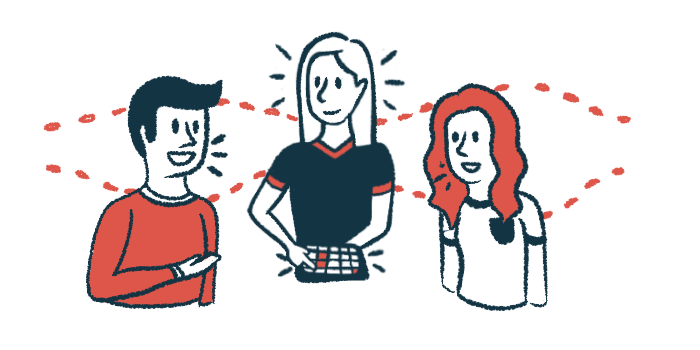
While best known for its role in breastfeeding and childbirth, oxytocin also helps regulate key aspects of human behaviors, including strengthening social interactions and interpreting emotional expressions.
In this study, a team led by researchers at the Danish Dementia Research Centre at Copenhagen University Hospital, Denmark hypothesized that reduced oxytocin levels could underlie, at least in part, early behavioral symptoms in Huntington’s patients.
The researchers measured oxytocin levels in the blood and cerebrospinal fluid, which surrounds the brain and spinal cord, from 113 patients with Huntington’s disease positive for expansion of CAG in the HTT gene and 33 family relatives without the gene’s expansion, who served as controls. All underwent a psychiatric and cognitive evaluation. Social cognition tests were also performed.
Oxytocin levels in the CSF were significantly lower — a mean reduction of 33.5% — in the Huntington’s group compared to controls, results showed. No differences were seen in blood samples from each group.
Researchers then divided the patients between those with clear motor manifestations and those without them, called premanifest Huntington’s. Only those with motor manifest Huntington’s disease retained the statistically significant difference relative to controls, a mean reduction of 37.8% in oxytocin levels in the CSF.
Although the premanifest Huntington’s patients also showed a lower level of oxytocin (mean reduction, 26.6%) than controls, it wasn’t statistically significant.
The team conducted the same analysis but took disease progression into account, assessing it using the Unified Huntington’s Disease Rating Scale (UHDRS) score and a disease burden score, called CAG age product (CAP), that takes into account the number of CAG repeats and age. No significant correlation was found between the two parameters and oxytocin levels, however.
These findings suggest that the level of oxytocin in the CSF “does not appear to be a surrogate marker of disease progression,” the researchers wrote.
Since their hypothesis focused on a potential link between oxytocin and non-motor symptoms, the researchers divided the Huntington’s disease group according to the presence of cognitive or psychiatric symptoms.
Oxytocin levels were significantly lower — by 30.3% — in those with cognitive impairments, results showed.
No differences were seen between patients without cognitive impairments and controls as well as patients with or without psychiatric symptoms.
Oxytocin as biomarker of social cognition
A significant positive correlation — meaning the greater one, the greater the other — was found between the level of oxytocin and patients’ scores on social cognition tests, namely the Reading the Mind in the Eyes (RME), the Emotion Hexagon test (EHt), and the Awareness of Social Inference Test (TASIT), which assesses social cognition using videos of everyday conversations between two actors.
This meant patients who fare worse at social interactions had lower levels of oxytocin, supporting the use of oxytocin levels as a potential biomarker of social cognition impairment.
The study showed Huntington’s disease patients “have a significantly lower level of oxytocin compared to controls and that the level of oxytocin may represent an objective and comparable measure that could be used as a state biomarker for impairment of social cognition,” the researchers wrote.
The results also suggest that administering oxytocin may improve social cognition in these patients.
“Our findings of a relationship between lower oxytocin levels in CSF and reduced social cognition in HD [Huntington’s disease] open up possibilities for treatment trials to evaluate potential effects of administration of oxytocin on social cognition in HD,” the researchers said.