Past Alcohol Abuse Linked to Motor, Psychiatric Problems in Patients
Written by |

wavebreakmedia/Shutterstock
A history of high alcohol intake seems to be linked to increased motor impairment and a higher burden of psychiatric symptoms in Huntington’s disease patients, a large international study suggests.
The observational study, “Genetic and Environmental Contributors to Neurodegeneration: An Exploration of the Effects of Alcohol on Clinical Features of Huntington’s Disease Using the Enroll-HD Global Platform,” was published in the International Journal of Environmental Research and Public Health.
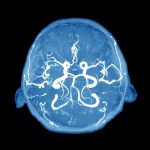
Huntington’s is a neurodegenerative disorder characterized by loss of cognitive ability, psychiatric problems, and motor impairments, including difficulty walking and maintaining balance, and chorea (uncontrolled jerking and writhing movements).
Common first symptoms include behavioral changes and psychiatric problems such as depression, which has been reported to affect half of patients. Irritability, aggression, and apathy are also frequent.
Evidence suggests that alcohol abuse is linked to disease onset. However, it remains unclear whether alcohol dependence is more frequent among Huntington’s patients. Psychiatric symptoms have also been shown to be more common among patients who misuse alcohol.
To investigate the impact of ongoing or past alcohol abuse and symptom onset in Huntington’s patients, a group of researchers at The Walton Centre NHS Foundation Trust, in the U.K., analyzed data from the international Enroll-HD study, which includes data from more than 16,000 patients diagnosed with Huntington’s or with an expansion in the HTT gene (premanifest), which will eventually lead to symptomatic Huntington’s.
In total, they analyzed data from 16,120 patients (7,393 men and 8,727 women), located across Europe, America, and Australasia (a region which comprises Australia, New Zealand, and some neighboring islands).
Most patients had manifest disease, and 5,173 were premanifest. For those who had manifest disease, symptom onset occurred at the age of 45.2 years, but the first visit to the clinic took place about 3.5 years later. Motor symptoms, including chorea, were the most frequent (52%) at disease onset, followed by psychiatric (21%) and cognitive symptoms (8%).
Current high alcohol intake — defined as greater than 30 units per week — was 3% in the combined premanifest and manifest population. However, 9% reported a history of alcohol problems in the past. This was more common in patients with manifest disease than in those with premanifest disease (7.7% vs. 2.3%).
A very small fraction of patients (0.6%) had both a past history of alcohol abuse and current high alcohol intake. Also, 12% of patients reported the use of recreational drugs.
There was no correlation between past alcohol use and the age at onset of symptoms. The proportion of patients with motor symptoms was similar between patients who drank a minimal amount of alcohol (37.2%), patients who had misused alcohol in the past (40.2%), and those currently misusing alcohol (41.2%).
However, patients with a history of high alcohol intake (30.7%) or those currently misusing it (55.3%) were more likely to have a psychiatric symptom as their first clinical feature compared to those who did not drink excessively (4.9%).
Patients who reported alcohol abuse in the past had a statistically significant increase in motor impairments, as assessed by their Unified Huntington’s Disease Rating Scale total motor scores. When compared to controls, those who reported excessive alcohol intake in the past had a significantly higher burden of psychiatric symptoms, including depression, irritability, psychosis, apathy, and executive function, as assessed by their Problem Behaviours Assessment scores. However, this was not observed for patients currently drinking excessively.
Individuals with a history of alcohol abuse, and those who currently consumed high levels of alcohol, had no cognitive impairment relative to those who did not report alcohol abuse, as assessed by the Mini-Mental State Examination.
The researchers reported a case of a female patient with no prior history of alcohol abuse, who developed impulsivity and compulsive behaviour, which led to excessive daily alcohol drinking. Her symptoms of aggression and impulsive behavior ultimately escalated, leading to an emergency admission for psychiatric assessment and treatment.
After this, the patient drastically changed her routines and focused her compulsion on exercise, rather than on drinking alcohol, with her family noting improvements in motor function and cognition, as well as diminished psychiatric disturbance.
“While we found that alcohol misuse in HD [Huntington’s disease] as a problem in a significant minority of the HD population, specific patterns were difficult to elucidate,” the researchers wrote.
“These results provide the clinician with an additional factor to address patients with problem alcohol use; in particular to be aware of more frequent depression, irritability and apathy and the value of counselling pre-manifest carriers of the HD genetic expansion about the risk of high alcohol intake,” they concluded.