Protein Identified That Protects Cells from Neurodegenerative Diseases, Possibly Leading to New Therapies
Written by |
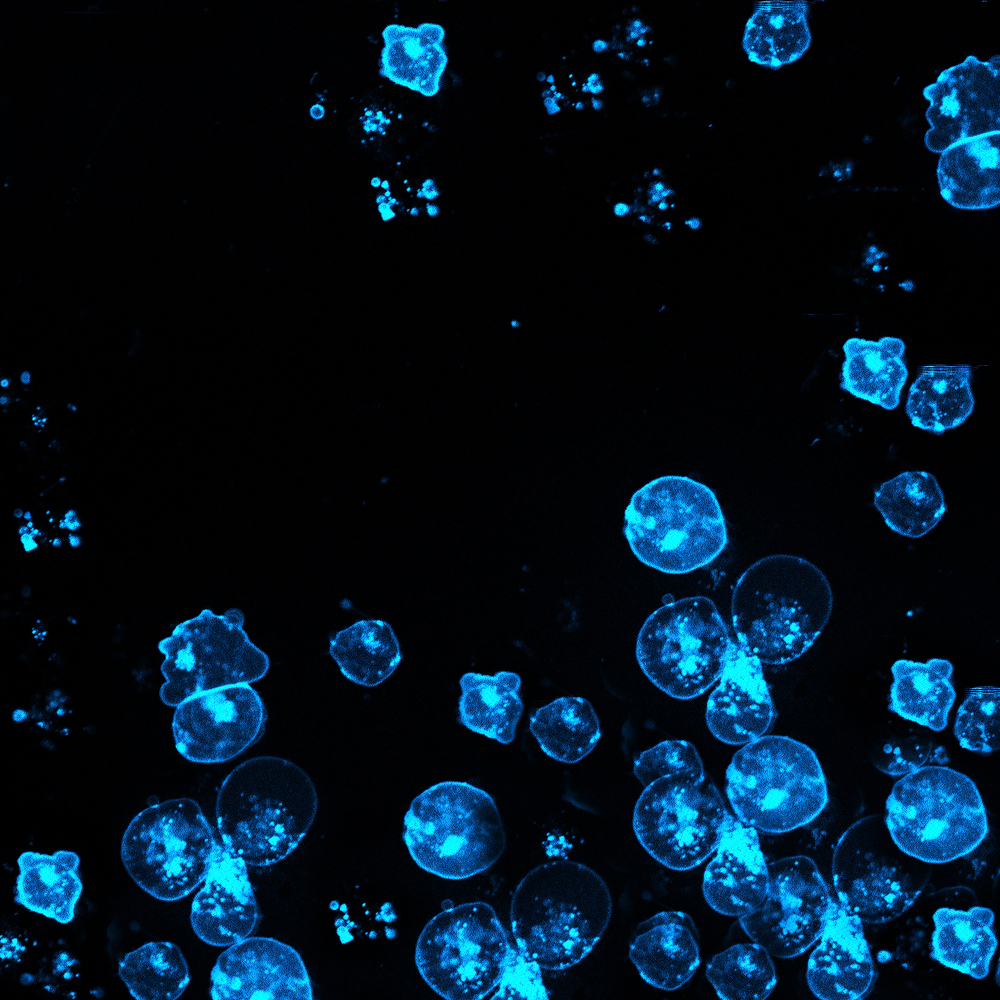
The accumulation of toxic protein aggregates within nerve cells are a hallmark of neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s, or Huntington’s disease. Now, researchers at the University of Glasgow in Scotland have identified a protein called UBQLN2 that protects against such diseases by eliminating those protein aggregates.
The study, “UBQLN2 Mediates Autophagy-Independent Protein Aggregate Clearance by the Proteasome,” published in Cell, may have revealed a new therapeutic target for neurodegenerative diseases.
As we age, the mechanisms that maintain the quality of our proteins become disrupted. As a result, proteins may become misfolded and accumulate in large, insoluble protein aggregates. Usually, these dangerous aggregates are cleared by UBQLN2, which detangles the aggregated proteins, eliminates misfolded proteins, and prevents future aggregate formation. But when this protein becomes mutated it can no longer remove these harmful aggregates, which may lead to neurodegenerative diseases.
“The function of UBQNL2 is connected to many neurodegenerative disorders, such as Parkinson’s, Alzheimer’s and Huntington’s disease,” Dr. Thimo Kurz, from the Institute of Molecular, Cell and Systems Biology, said in a press release.
“These patients often have very clear clumps in their brain cells. Using mice that mimic human Huntington’s disease, we found that when UBQLN2 is mutated, it could no longer help nerve cells to remove protein clumps in the brains of these mice,” Kurz said.
Previous work had shown that mutations in the UBQLN2 gene led to a neurodegenerative disease called amyotrophic lateral sclerosis with frontotemporal dementia (ALS/FTD or motor-neuron disease with dementia). However, until now researchers did not know how mutations in UBQLN2 could lead to the development of this disease.
Now that the team understands how UBQLN2 mutations can lead to the development of neurodegenerative diseases, new research may lead to the development of novel therapeutic options for patients with such diseases.
“The significance of this discovery goes beyond the role of UBQLN2 in motor-neuron disease with dementia,” said Dr. Roland Hjerpe.
“Our study has revealed a new mechanism by which nerve cells cope with protein clumps in general, which has implications for most neurodegenerative diseases and can open up avenues for new therapeutic interventions to treat these conditions in the future,” he said.





