Endurance Training May Delay Muscular Dysfunction in Huntington’s Patients, Study Shows
Written by |
Huntington’s disease (HD) patients respond to endurance training much like anyone else, by increasing muscular energy metabolism, say Swiss researchers who suggest such training might help delay muscular dysfunction in patients.
Their study, “Effects of endurance training on skeletal muscle mitochondrial function in Huntington disease patients,” appeared in the Orphanet Journal of Rare Diseases.
HD is a progressive neurodegenerative disorder caused by mutations in the gene encoding the huntingtin protein. This protein is found in most tissues, including the skeletal muscle. Despite significant research on the role of huntingtin in the central nervous system, information on its role in skeletal muscle is scarce.
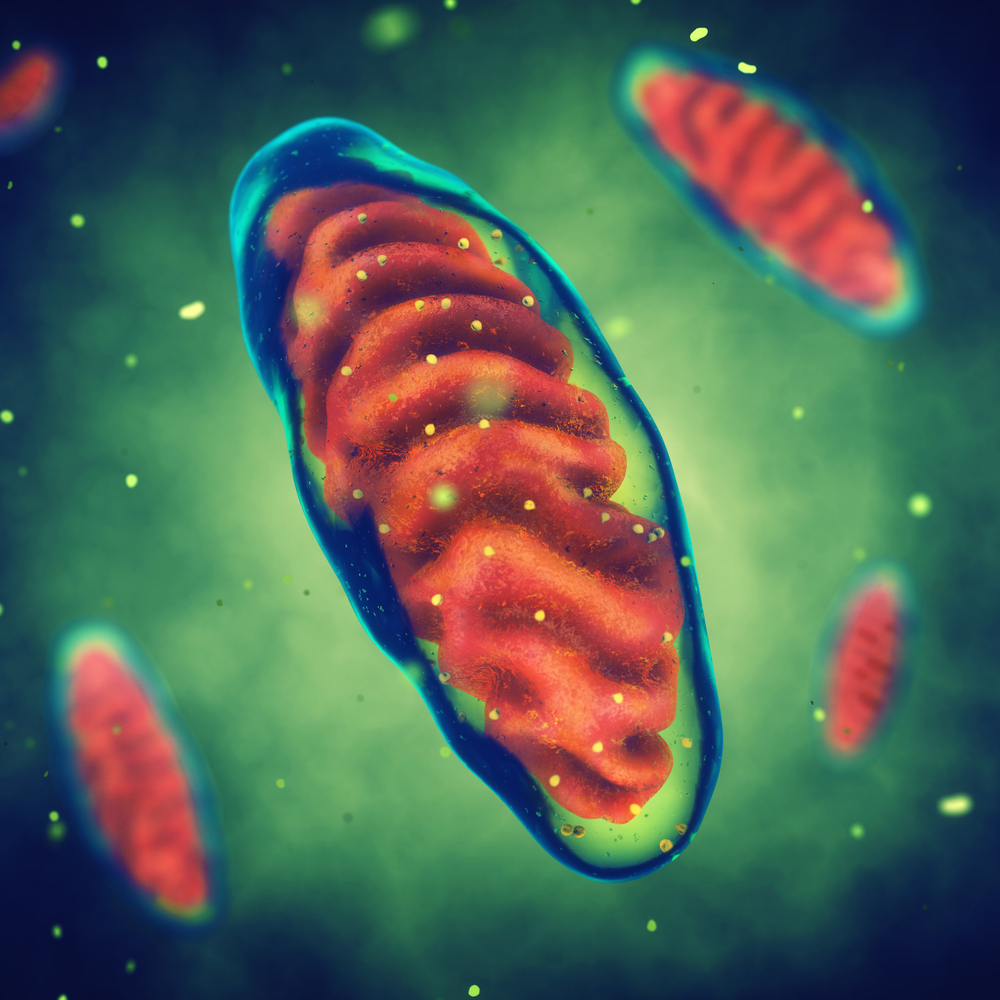
Research suggests that abnormal functioning of mitochondria in the skeletal muscle may be a pathogenic factor in HD.
Physical activity improves mitochondrial function in healthy subjects, while the benefits of physical exercise on coordination, gait, motor symptoms and HD progression have been shown in mice. Furthermore, endurance training increases peak oxygen uptake similarly in HD patients and healthy controls. However, evidence of the benefits of physical exercise in the skeletal muscle of HD patients is still lacking.
Investigators at the University of Zurich hypothesized that although HD patients have impaired mitochondrial function in the skeletal muscle, endurance exercise could improve it to a similar extent as in healthy controls.
The study (NCT01879267) included 13 HD patients and 11 healthy controls. First, researchers observed the natural development of the disease for 26 weeks and then, assigned 26 weeks of endurance training to both HD and control groups. Exercise protocols comprised three phases, with one-week rest periods in between.
Researchers collected muscle biopsies from M. vastus lateralis (a muscle located in the thigh) before and after the training phase. Then they measured mitochondrial respiration parameters in a subgroup of six HD patients, including the activities of respiratory chain complexes — which transfer electrons sequentially and are linked to energy production — as well as mitochondrial respiratory capacity. In addition, they determined muscle capillarization, which is the density of capillaries supplying a muscle with oxygen, as well as fiber type distribution
Results showed that the activities of the enzyme citrate synthase (a mitochondrial matrix marker), and of the electron transport complexes succinate cytochrome c reductase, Complex III, and Complex V (parts of the energy-producing complex in the mitochondria) increased similarly during training in both groups.
HD patients exhibited lower pre-training citrate synthase activity than did controls. However, in HD patients, exercise increased this activity to values equivalent to the pre-training measurements of healthy controls.
HD patients further boosted their mitochondrial respiratory capacity during the endurance training intervention. In addition, exercise augmented the overall capillary-to-fiber ratio in HD patients (8.4%) and healthy controls (6.4%). A higher ratio means better blood innervation of the muscle tissue. In contrast, no change was observed in muscle fiber type in either group.
The findings demonstrate that endurance training induces a similar response in skeletal muscle mitochondria of HD patients and healthy controls, said authors, concluding that “endurance training is a safe and feasible option to enhance indices of energy metabolism in skeletal muscle of HD patients and may represent a potential therapeutic approach to delay the onset and/or progression of muscular dysfunction.”


