In Huntington’s Disease, Calcium Overload Leads to Mitochondrial Dysfunction and Cell Death
Written by |
Researchers at Philadelphia’s Thomas Jefferson University investigated the physiological and pathological role of MICU1 (Mitochondrial Calcium Uptake 1), a protein that controls calcium by the mitochondria, a process involved in cell survival.
Results suggest that strengthening this protein’s function and inhibiting mitochondrial calcium uptake could be a novel therapeutic approach to the treatment of several diseases, including Huntington’s disease, in which mitochondrial damage is found to exacerbate neurodegeneration.
The research paper, “MICU1 regulation of mitochondrial Ca2+ uptake dictates survival and tissue regeneration,” was published in Nature Communications.
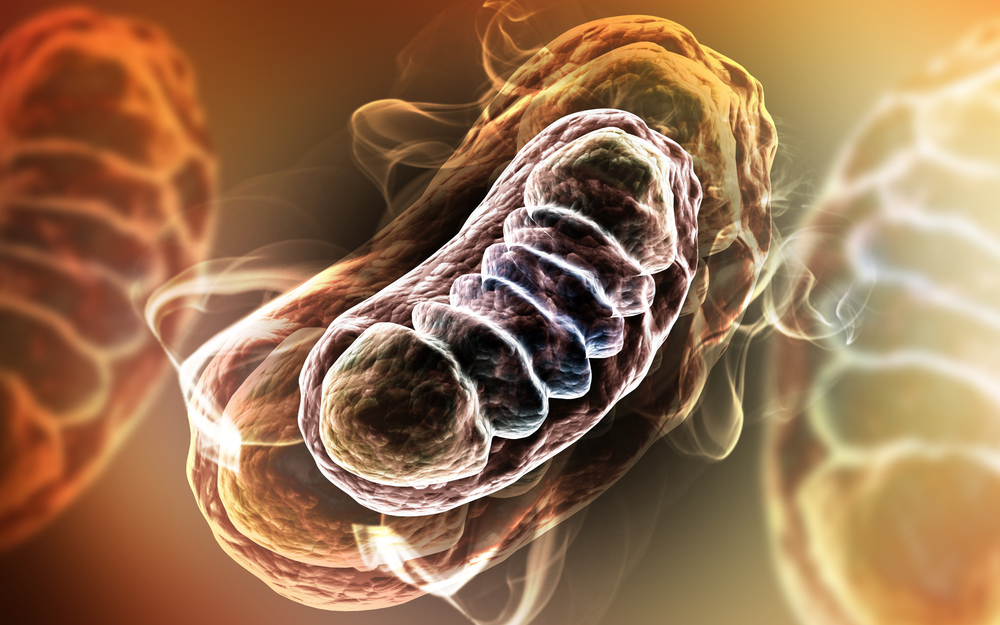
Mitochondrial failure and damage is associated with cellular and tissue injury observed in many conditions, such as strokes and heart attacks. Such dysfunction is especially alarming in organs like the liver, heart, and brain, which are extremely energy dependent. Energy deficits or other types of stress can lead to the accumulation of calcium in cells and, specifically, inside the mitochondria, which ultimately can result in cell death.
Mitochondrial dysfunction and calcium overload, while not the pathogenic drivers of disease, have also been shown to be involved in the progression of neurodegenerative diseases, such as Alzheimer’s and Huntington’s disease. Scientists at the MitoCare Center at Thomas Jefferson University had shown, in previous research studies, that MICU1 controls mitochondrial calcium uniporter (MCU), preventing continuous calcium intake, but still allowing calcium signals in to allow energy production.
Researchers, seeking to understand the physiological and pathological role of the protein MICU1, developed the first animal model lacking the protein. The scientists observed that these mice developed normally in utero but died soon after birth, suggesting that MICU1 is vital to postnatal life.
Researchers removed the protein only in the liver of mice and found that, while liver function was normal, when stress was induced — in this case removal of part of the liver — the organ failed to regenerate as it normally does. Researchers observed that such response was a result of too much calcium overload into cellular mitochondria, which led to cellular death.
“Inhibiting mitochondrial calcium uptake as a short-term treatment could offer real promise for acute heart and brain attacks,” said Prof. György Hajnóczky, M.D., Ph.D., the study’s senior author and director of the MitoCare Center, in a news release. “It remains unpredictable in complex and chronic neurodegeneration whether a simple inhibition of calcium uptake would be effective. Rather, strengthening both the sophisticated gatekeeping as well as the calcium signaling function of MICU1, might be sensible.”


