Gut Microbiome Seen to Differ in People With Huntington’s or at Disease Risk
Written by |
Microbes in the gut of people with Huntington’s or likely to develop this disease appear to differ from healthy peers, opening the door to potential new biomarkers and therapeutic targets, according to a recent study.
The study, “Gut dysbiosis in Huntington’s disease: associations between gut microbiota, cognitive performance and clinical outcomes,” was published in the journal Brain Communications.
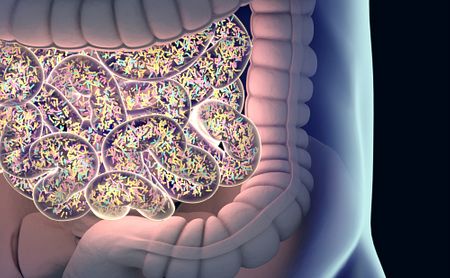
The trillions of microbes that populate the human gut — collectively known as the gut microbiome — moderate communication between the gut and the brain.
Harmful alterations in their composition, a process called dysbiosis, have been implicated in several neurodegenerative diseases — from multiple sclerosis and amyotrophic lateral sclerosis to Parkinson’s and Alzheimer’s — and was recently found in a mouse model of Huntington’s.
Researchers at Monash University and the Florey Institute for Neurosciences, both in Australia, investigated whether the gut biomes of Huntington’s gene expansion carriers might differ from those of healthy people.
They compared 42 patients, 19 diagnosed with Huntington’s and 23 who were in the premanifest stage (those with identified mutations but not yet showing symptoms), with 36 age- and sex-matched healthy controls.
Patients had a total functional capacity range of 6 to 13, as measured by the Functional Capacity domain of the Unified Huntington’s Disease Rating Scale. This domain is used to measure items related to capacity to work, perform domestic chores, self-care, or the ability to live independently. Higher scores, on a 0 to 13 scale, indicate better functioning and greater independence.
The gut microbiomes of Huntington’s patients were found to differ considerably from those of healthy participants.
Overall, patients’ gut microbiomes appeared to be populated by fewer microbial species, making for a less rich environment.
In particular, a bacterial species called Eubacterium hallii associated with several clinically relevant characteristics of Huntington’s.
Symptomatic patients with low numbers of E. hallii tended to show more severe motor symptoms. Presymptomatic individuals had a strong and negative correlation between the abundance of E. hallii and the time of symptom onset. In other words, the lower the numbers of E. hallii in their microbiome, the more quickly they are expected progress to evident symptoms.
E. hallii also associated with declines in memory performance, although the study’s authors noted these results should be treated with caution, given the low number of people in the study and the simultaneous presence of other non-significant correlations.
Differences between men with and without Huntington’s appeared to be greater than these female groups, leading the investigators to speculate that sex could interact with the relationship between gut microbes and Huntington’s progression.
Several of the differences observed between the Huntington’s group and healthy controls might affect the metabolism of certain amino acids (the building blocks of proteins), such as methionine. The researchers suggested these changes could be important, since methionine links to oxidative stress, which may contribute to neuroinflammation and disease-related damage to the brain.
Of note, oxidative stress occurs when there is an imbalance between the production of free radicals and the ability of cells to detoxify them. These free radicals, or reactive oxygen species, are damaging to cells.
This finding “raises interesting questions about the possibility of future development of gut biomarkers,” the researchers wrote.
“Homeostasis of the gut microbiome is important for human health, and influences behaviour and brain function via the gut-brain axis,” they continued. “Thus, some of the clinical manifestations or brain changes evident in Huntington’s disease may be related to a gut-driven modulation of brain inflammatory pathways.”
As the first study to find evidence of gut dysbiosis in people with Huntington’s, it highlights the importance of better understanding how the gut fits into the progression of Huntington’s.
“[T]hese results raise the tantalising proposition of whether the gut may be a potential target for future therapeutic intervention to improve outcomes in Huntington’s disease and other neurodegenerative diseases,” the researchers concluded.


