New Virus Variant May Advance Gene Therapy for Diseases Like Huntington’s
Written by |
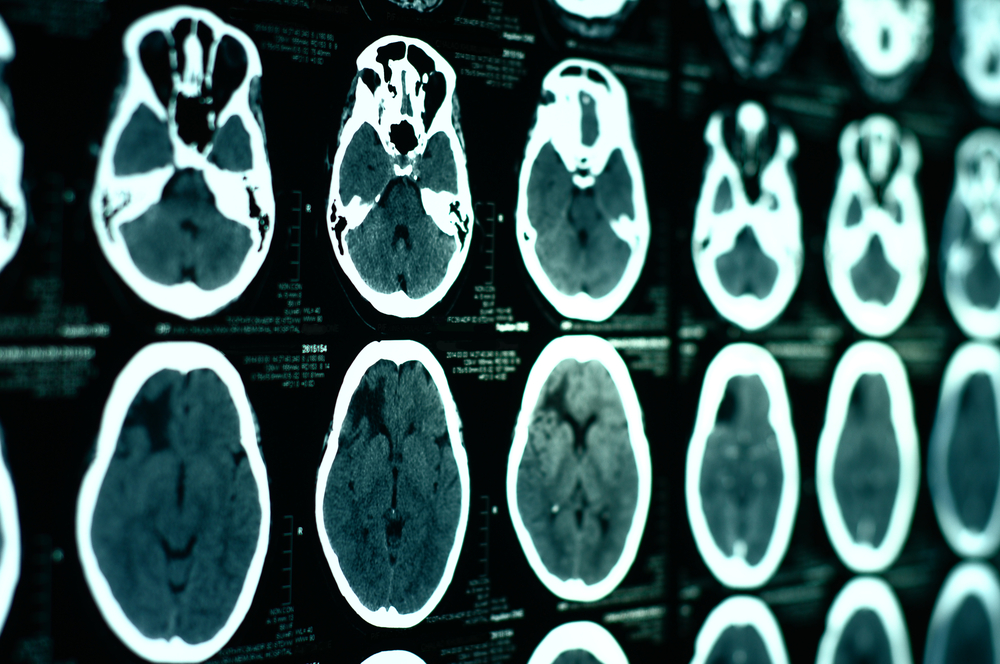
A research team successfully developed a virus variant that is more efficient than the current standard at crossing the blood-brain barrier and delivering genes to the central nervous system (CNS), making it a promising gene therapy approach to treating neurodegenerative diseases such as Huntington’s disease.
The blood-brain barrier, made up of specialized and tightly packed endothelial cells, forms a semi-permeable barrier that separates the brain from the circulatory system, both protecting it from harmful pathogens and maintaining a balanced environment for the proper functioning of the CNS. Its very effectiveness, however, makes it difficult for drugs and other molecules to be delivered to the brain via the bloodstream. Various approaches have been used over two decades of research, and scientists were able to deliver AAV9, a strain of the adeno-associated viruses (AAVs), to the brains of neonatal or infant mice via the bloodstream in 2009, but not to adult mice.
“The big challenge was how do we achieve the same efficiency in an adult,” Viviana Gradinaru, assistant professor of biology and biological engineering at Caltech and senior study author, said in a Caltech press release. The study, “Cre-dependent selection yields AAV variants for widespread gene transfer to the adult brain,” was published in Nature Biotechnology.
Because the number of variables that govern any single virus’ behavior is very high, the Caltech researchers had to develop a method that would allow them to test millions of virus variants in vivo, and select the ones most efficient at entering the brain and delivering genes to a specific type of brain cells, astrocytes. They named their method CREATE, for Cre REcombinase-based AAV Targeted Evolution.
Starting with the AAV9 virus, the researchers produced millions of viral variants, that were then injected intravenously into adult mice that only expressed the Cre enzyme in the astrocytes. The interaction of this enzyme with the specially designed viruses allowed scientists to identify and recover variants that successfully transferred the gene into the target cell. The researchers then repeated the selection process and identified one variant, which they named AAV-PHP.B, as a top performer. Finally, the team assessed its efficiency to enter the brain, spinal cord, and retina in adult mice, using AAV-PHP.B to deliver a gene that codes for a protein that glows green and is easy to visualize in cells expressing it.
The results showed that AAV-PHP.B was expressed in the CNS with a high level of efficiency, and its gene delivery was 40 times more efficient than AAV9.
“What provides most of AAV-PHP.B’s benefit is its increased ability to get through the vasculature into the brain,” said Ben Deverman, lead study author. “Once there, many AAVs, including AAV9, are quite good at delivering genes to neurons and glia.”
Researchers believe the CREATE platform could be useful to produce customized AAV vectors for biomedical applications. For neurodegenerative diseases, especially, the platform could be a first step in a promising therapy strategy. “Many disorders are not tightly localized. Neurodegenerative disorders like Huntington’s disease affect very large brain areas. Also, many complex behaviors are mediated by distributed interacting networks,” Dr. Gradinaru said. “Our ability to target those networks is key in terms of our efforts to understand what those pathways are doing and how to improve them when they are not working well.”
Gene therapy commonly uses AAVs to deliver genes into the nuclei of cells where they can be expressed. In some applications, the genes replace nonfunctional gene copies responsible for disease, while in others, the genes delivered generate antibodies or fluorescent proteins to aid research.


