CHOP Researchers Restore Cellular Energy Signals, Offering Possibility of Treating Mitochondrial Diseases
Written by |
Mitochondrial disorders are complex conditions for which few treatments are available. Now, using microscopic worms, researchers at The Children’s Hospital of Philadelphia (CHOP), are researching if existing human drugs aimed at improving metabolism and restore shortened lifespans, can open the opportunity for human clinical trials on innovative therapies for these conditions. The study is published in journal Mitochondrion.
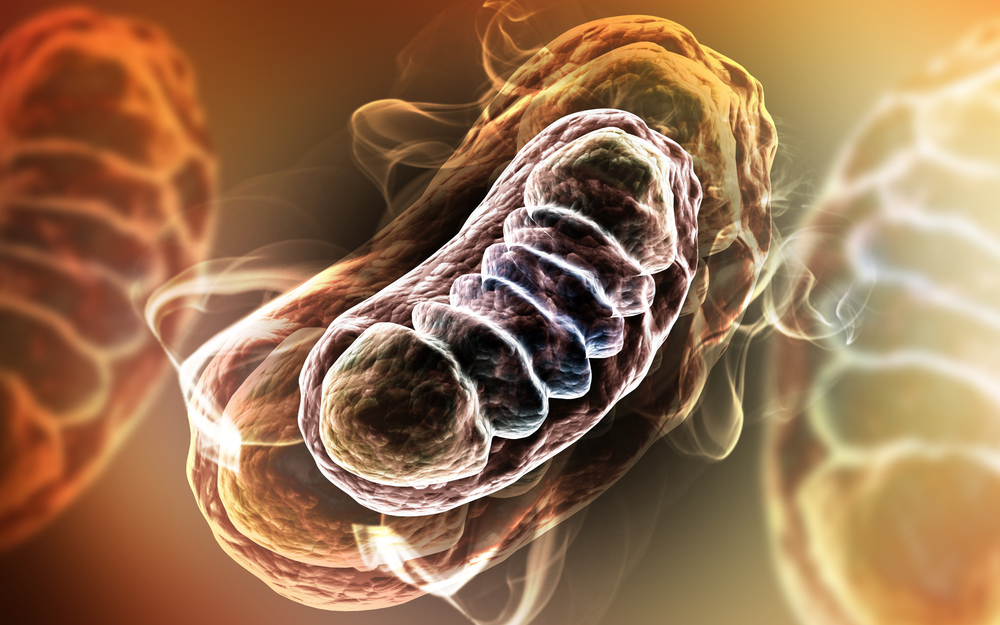
Mitochondria are the power plants of the human cell and use oxygen to create energy from the food we eat. They produce about 90 percent of the energy the body uses. Dysfunctional mitochondria fail to produce enough energy for cell function and can cause the body to have a “power shortage.” This shortage can affect organ function in any system of the body. As a result, mitochondrial disease takes many forms and is difficult to diagnose.
Primary mitochondrial conditions are rare, but has there are hundreds of these disorders, they collectively affect at least one in 5,000 individuals. Mitochondrial dysfunctions also play a role in conditions such as epilepsy, type 2 diabetes, Alzheimer’s disease, and even human aging.
“This work carries strong promise for identifying effective therapies for mitochondrial diseases,” said study leader Marni J. Falk, M.D., director and attending physician in the Mitochondrial-Genetic Disease Clinic at The Children’s Hospital of Philadelphia (CHOP) in a recent news release. “The drugs we used in this study improve cellular signaling in ways that could directly benefit patients. As all but one of the drugs are currently prescribed for other diseases, they’re already available to now test in clinical trials in patients with mitochondrial disease.”
The research team focused their work on the respiratory chain, a set of five enzyme complexes that produce energy inside the mitochondria. Defects in the respiratory chain (RC), are common in mitochondrial disorders, and cells do not produce energy.
RC dysfunction is usually located in a group of proteins called complex 1, where usually occurs a key metabolic product, called nicotinamide adenine dinucleotide (NAD+). NAD+ is responsible for the regulation of other chemical reactions within the cell. However, when genetic mutations affect the proteins of the complex 1, patients suffer energy shortages in the brain, eyes, heart, muscles, as well as in many other parts of the body.
In the new research, the scientists used microscopic worms with genetic mutations that disrupt their mitochondria. Using these worms, named, called Caenorhabditis elegans, Falk’s research group has already conducted many studies on mitochondrial diseases and potential treatment strategies.
In this new study, they evaluated a series of drugs for the treatment of diabetes or lipid disorders. One of the drugs that researchers used, called nicotinic acid, is a type of vitamin B3 widely used as treatment in people with high triglycerides blood concentrations.
The worms used in the study had mutations that directly impaired their complex I function and reduced their lifespans. Results revealed that Nicotinic acid was able to restore the animals’ lifespans, and was also able to restore the levels of NADH, thus enabling NADH to function as appropriately produce cellular energy, and also to regulate other cellular processes.
Results also revealed that other available human drugs also improved key metabolite levels inC. elegans. “In contrast to research that aims to repair defective mitochondria, we are bypassing the damaged mitochondria and focusing instead on how cells respond to mitochondrial problems,” said Falk in the news release. “We’re restoring the ratio of critical metabolic precursors and products that control signaling pathways, thereby improving overall cellular health in respiratory chain diseases.”
According to Falk, mitochondrial disorders are highly complex, but the team nematode researches have revealed central conserved processes that are disrupted in mitochondrial disease, has they were able to recognize many of the biological mechanisms resulting of changes in oxidant levels, genome expression patterns and other major physiological effects.
“Although some specific mechanistic details may differ, we’re looking at how the effects of different drugs may converge to promote an organism’s health and survival,” she said in the news release.
The research team is now working in a pilot trial in children affected with complex 1 abnormalities in order to understand if the results seen in animals also apply to human patients.
“We’re enthusiastic that we have reached a major threshold on the path toward bringing important new therapies to a very challenging group of diseases,” she added in the news release.


