Huntington’s Patients, with Disease and Premanifest, Show Similar Metabolic Profile
A study with a small cohort of Huntington’s disease patients differed from previous research in finding no metabolic alterations associated with disease progression in stage 2/3 patients compared to both premanifest and healthy subjects. The study, titled “A Metabolic Study of Huntington’s Disease,” was published in the PLOS One journal.
Huntington’s disease, an inherited and neurodegenerative genetic disorder, impairs movements and cognition, and leads to mental decline and behavioral symptoms. Increasing studies suggest that Huntington’s is a systemic disorder, affecting multiple organs and tissues, so that its pathology is not detected within the brain. Symptoms of Huntington’s peripheral pathology, including weight loss and alterations in appetite, are possibly linked to endocrine and metabolic alterations.
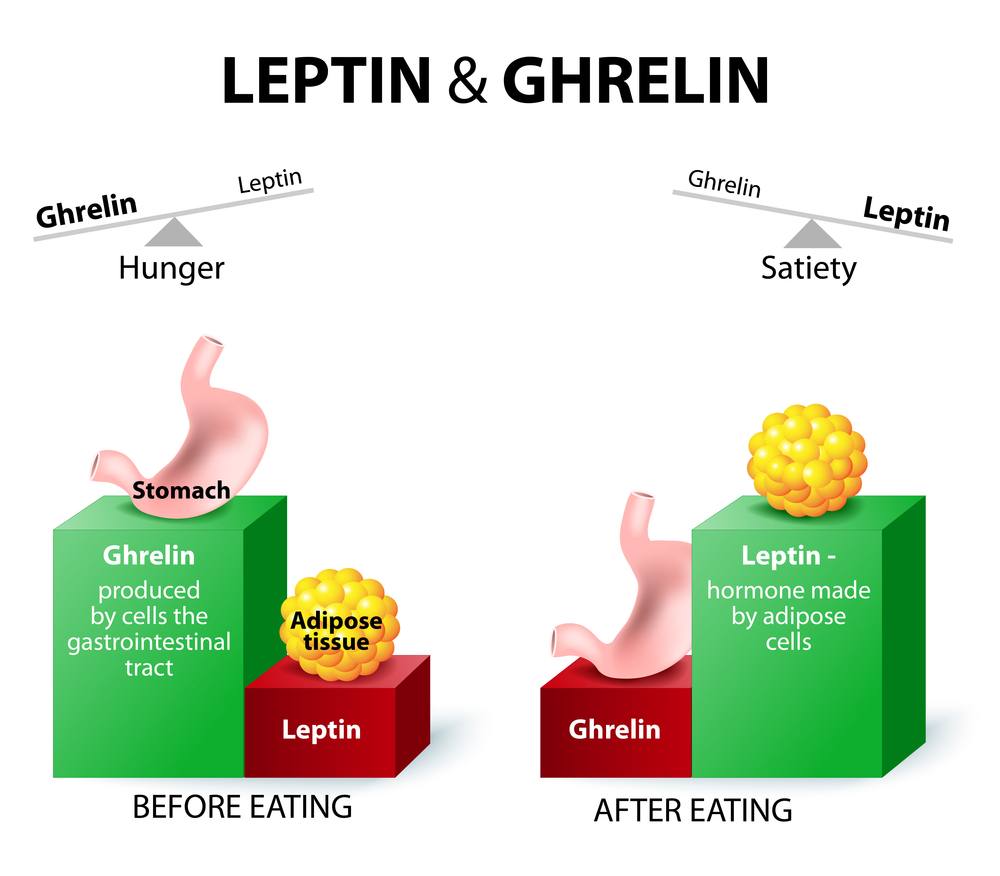
UCL Institute of Neurology researchers investigated whether Huntington’s disease patients exhibit metabolic and endocrine abnormalities, marked by carbohydrate, lipid, or protein metabolites and/or hormones related to energy metabolism alterations. The team analyzed blood samples collected within a 24-hour period from controls (n=15), and from premanifest (n=14) and stage 2/3 Huntington’s disease patients (n=13), and quantified fasting baseline concentrations of glucose, insulin, cholesterol, triglycerides, lipoprotein (a), fatty acids, amino acids, lactate and osteokines. Both leptin and ghrelin levels were measured before and after meal.
Researchers found no significant alterations in carbohydrate, protein or lipid metabolism levels in the three groups. While other marker levels, including osteoprotegerin, tyrosine, lysine, phenylalanine and arginine, were slightly higher in patients with premanifest Huntington’s, researchers attributed no significance to these levels.
The analysis performed in this study was restricted to Huntington’s patients not taking neuroleptics, anti-depressants or other medications that affect metabolic pathways and, contrary to many previous studies, researchers found no significant evidence of metabolic alterations linked with Huntington’s progression. However, the research team noted a few limitations to its study: the exclusion of more severe patients (those on neuroleptic and other medication), premanifest subjects who had a higher BMI compared to controls, and the small size of cohorts (a maximum of 15 subjects). These preliminary findings require follow-up studies with a larger sample size for more definitive conclusions.