CHDI Foundation Award to Advance Research in Huntington’s Disease
Written by |
The CHDI Foundation, a privately-funded nonprofit research organization dedicated to fighting Huntington’s disease, has awarded a research grant to a team of scientists from the University of Rochester Medical Center (URMC) to study the role of specific cells in the development of the disease.
Dr. Steve Goldman, MD, PhD, co-director of URMC’s Center for Translational Neuromedicine, will lead the team. The funding is anticipated to cover $10.5 million over the next five years.
According to a press release, the award will help advance a research project based on findings Goldman and his team published earlier this year showing that disease progression slowed in mice when healthy human support cells – called glial progenitor cells – were transplanted into the brains of mice with Huntington’s disease.
These findings were published in the journal Nature Communications in an article titled “Human glia can both induce and rescue aspects of disease phenotype in Huntington disease.”
With the new funding, researchers hope to dig deeper into the basic biology of glial cells so they can refine the process of preparing them for implantation before continuing to human clinical trials.
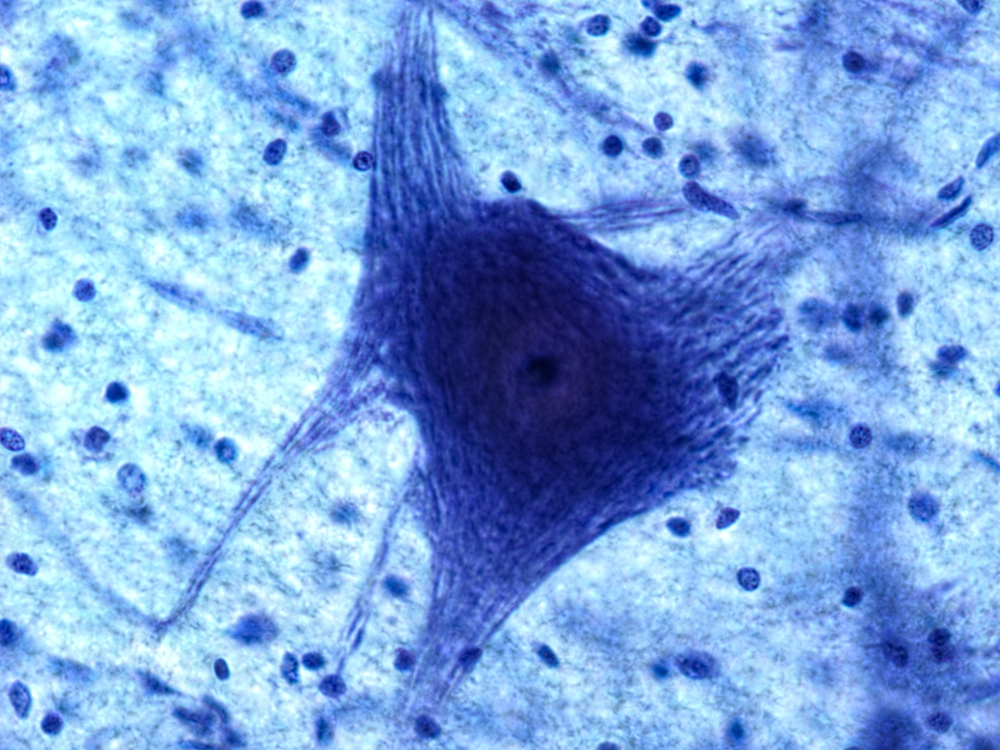
Glial cells are non-neuronal cells that sustain stability, form myelin (the fatty substance that covers nerve fibers), and provide support and protection for neurons in the central nervous system (CNS) and in the peripheral nervous system (PNS). One of main roles of glial cells is to help medium spiny neurons maintain a balanced supply of potassium.
A genetic flaw caused by Huntington’s keeps cells from absorbing enough potassium. This deficit leads not only to motor control and cognitive symptoms, it also triggers a toxic chain reaction responsible for eventually killing the cells and accelerating disease progression.
“The role that glia cells play in the progression of Huntington’s disease has never really been explored,” Goldman said in a press statement released earlier this year.
Goldman and his team found that once the new glial cells took over, they were capable of stabilizing and even bringing back neurons that were being lost to the disease, successfully slowing the progression of the disease and allowing the mice to live longer.
These findings indicate that glial cell dysfunction plays a major role in the development of Huntington’s, which might pave the way to finding new treatments.
“This study shows that these cells are not only important actors in the disease, but may also hold the key to new treatment strategies,” Goldman said.


