Huntington’s Disease May Start Very Early in Embryo, Research Reveals
Huntington’s symptoms may be a late manifestation of a disease that begins much earlier in embryonic development, according to a recent study.
The research, “Chromosomal instability during neurogenesis in Huntington’s disease,” published in the journal Development, corroborates the idea that a lack of the huntingtin protein — not an excess of it — is driving the disease.
Huntington’s disease is caused by a mutation in the huntingtin (HTT) gene that takes the form of extra DNA and leads to the production of a longer-than-normal protein. The DNA itself is present in the form of a repeating sequence; the more repeats there are, the earlier the disease sets in.
Traditionally, Huntington’s has been thought of as an adult disease as symptoms and death usually occur during midlife. However, emerging studies have suggested that huntingtin has an important role in the developing brain, indicating that Huntington’s disease pathogenesis might start during embryogenesis.
Unfortunately, neither the mechanisms that lead to the disease nor the normal function of the huntingtin protein are well understood.
Currently, research heavily relies on animal models of the disease, which has left many questions unanswered. So, researchers at Rockefeller University used the gene-editing technology CRISPR — a powerful tool to easily alter DNA sequences and modify gene function — to engineer human embryonic stem cell lines with different numbers of DNA repeats at the ends of their HTT genes.
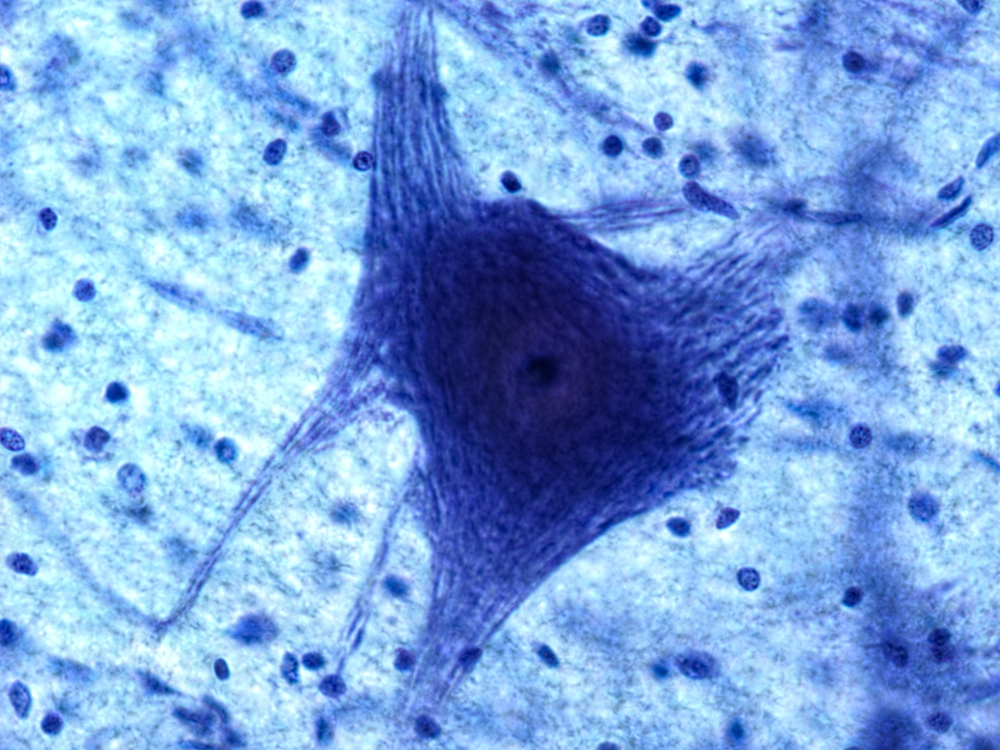
When these stem cells were pushed toward becoming neurons, a process called neurogenesis, researchers discovered a new developmental Huntington’s phenotype— the appearance of giant neurons with multiple nuclei, in contrast to normal neurons that are smaller and have only one nucleus.
Importantly, the more repeats in the mutation, the more multi-nucleated neurons appeared.
“We started seeing things that were completely unexpected,” Ali Brivanlou, PhD, lead author of the study said in a press release. “In cell lines with mutated HTT, we saw giant cells. It looked like a jungle of disorganization.”
“Our research supports the idea that the first domino is pushed soon after fertilization,” Brivanlou added, “and that has consequences down the line. The final domino falls decades after birth, when the symptoms are observable.”
Next, to determine the normal function of the huntingtin protein the team engineered cell lines that completely lacked the HTT protein. Interestingly, the same phenotype that was observed in cells with expansions of the HTT gene was seen in cells lacking the protein.
Researchers hypothesize that perhaps a lack of normal HTT protein, rather than the presence of the mutant HTT protein, is what causes the Huntington’s disease phenotype.
This is a departure from previous thinking because most drugs are targeted to eradicate mutant HTT protein from the brain.
“We should rethink our approach to treating Huntington’s,” Brivanlou said. “Both the role of the HTT protein and the timing of treatment need to be reconsidered; by the time a patient is displaying symptoms, it may be too late to medicate. We need to go back to the earliest events that trigger the chain reaction that ultimately results in disease so we can focus new therapies on the cause, not the consequences,” he said.
Researchers are hopeful that their new cell lines can be used to further study the intricacies of Huntington’s disease.






