Researcher Hopeful, Sure of Future Cure for Huntington’s Disease
Written by |
Edward J. Wild, of the National Hospital for Neurology & Neurosurgery, London, has a unique perspective on Huntington’s disease (HD). He believes the currently incurable neurological condition is ideal for certain treatment, based on the clear and universal cause of the disease.
Wild elaborated on his conviction in a recent article titled “Huntington’s Disease: The Most Curable Incurable Brain Disorder?“ and published in the June 2016 issue of EBioMedicine.
HD is caused by a well-understood mutation in the HTT gene, which causes the amino acid glutamine to repeat itself over and over in the protein coded by HTT, known as huntingtin.
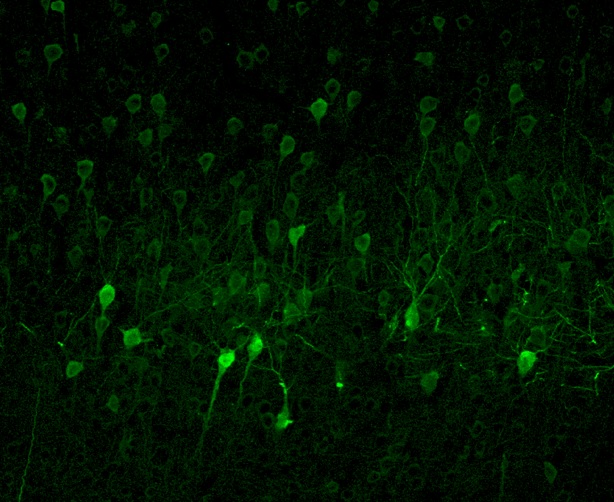
More repeats mean worse Huntington’s disease, an effect that can be reliably predicted by tests measuring how many glutamines in a row occur in the huntingtin protein. Unlike other degenerative conditions of the brain such as Parkinson’s and Alzheimer’s disease, Huntington’s always has the same genetic cause. Everyone who has the mutation will develop HD and widespread brain cell death, causing progressive problems with cognition, movement, and severe psychological symptoms.
Emphazing the irony of a clear cause with no current cure Wild said: “History has shown HD is an easy problem to define, for which it is surprisingly difficult to find solutions.”
So far already, FDA-approved drugs known to protect neurons have not successfully halted the disease’s toxic course: riluzole and minocycline, baclofen and lamotrigine. Likewise, neuron-protecting nutritional supplements such as creatine, coenzyme Q, and fish oil, haven’t helped either.
Still, Wild is optimistic. He believes that studies provide information needed to move the field forward.
“A failed drug does not imply a failed trial. Collectively, these experiences improved the field’s ability to design and run trials that can give a definitive answer, and to prioritize therapeutic targets and generate comprehensive preclinical data to inform decisions about advancing to clinical trials,” he wrote.
Notably, researchers have recently attempted to reduce the toxic form of huntingtin protein by interfering with the aberrant huntingtin gene using a blocker called IONIS-HTTRx, in what is called an “antisense” treatment that prevents the gene from being coded into protein by the intermediary known as mRNA.
The investigators used genetically-modified mice engineered to develop an experimental form of HD. The drug successfully improved HD-like movement problems in mice. In monkeys, IONIS-HTTRx reduced abnormal HTT mRNA and protein. The medication produced tolerable side-effects in the animals and was considered to be safe.
IONIS-HTTRx is currently in Phase 1 and 2 clinical trials and is set to begin testing in humans. It will be given through the cerebrospinal fluid in an increasing dose, in order to bypass the “blood brain barrier” — a biological checkpoint that stops many medications from getting into the central nervous system. The study will examine whether the drug is safe and tolerable, and collect initial information about its effects on HD.
Although the trials will take years, Wild notes that lowering huntingtin is an enormous leap forward toward treating HD — a condition he deems ultimately curable.