Combined Stem Cell, Gene Therapies Ease Symptoms, Prolong Survival in HD Mouse Model
Combining stem cell and gene therapy can ease symptoms and lengthen survival time in a mouse model of Huntington’s disease, according to recent research.
The study, “Combination of stem cell and gene therapy ameliorates symptoms in Huntington’s disease mice,” was published in the journal Regenerative Medicine.
Huntington’s is caused by a mutation in the huntingtin gene, which ultimately leads to brain cell (neuron) death. So, broadly, replacing these dying neurons with new neurons without the disease-causing mutation could be a way of eventually curing Huntington’s.
This is the basic idea behind stem cell therapy: stem cells are cells that can grow into other kinds of cells, a process called differentiation.
Particularly exciting in recent years is a type of stem cell called an induced pluripotent stem cell (iPSC). Stem cells that naturally occur in the body can be hard to access, and adults don’t have many. iPSCs are stem cells that are reverse-engineered from other kinds of cells, such as skin cells. This means that, at least in theory, clinicians could treat patients with iPSCs generated from the patient’s own cells. This removes the need for invasive collection and lowers the likelihood of the immune system attacking these cells.
For Huntington’s, though, this strategy comes with a key problem: if the stem cells used for treatment are iPSCs derived from a patient’s cells, those cells will have the same mutations as the patient — so they’ll also have the huntingtin mutation.
But what if the stem cells could be engineered not to make the mutated huntingtin protein? That is the idea behind the new study.
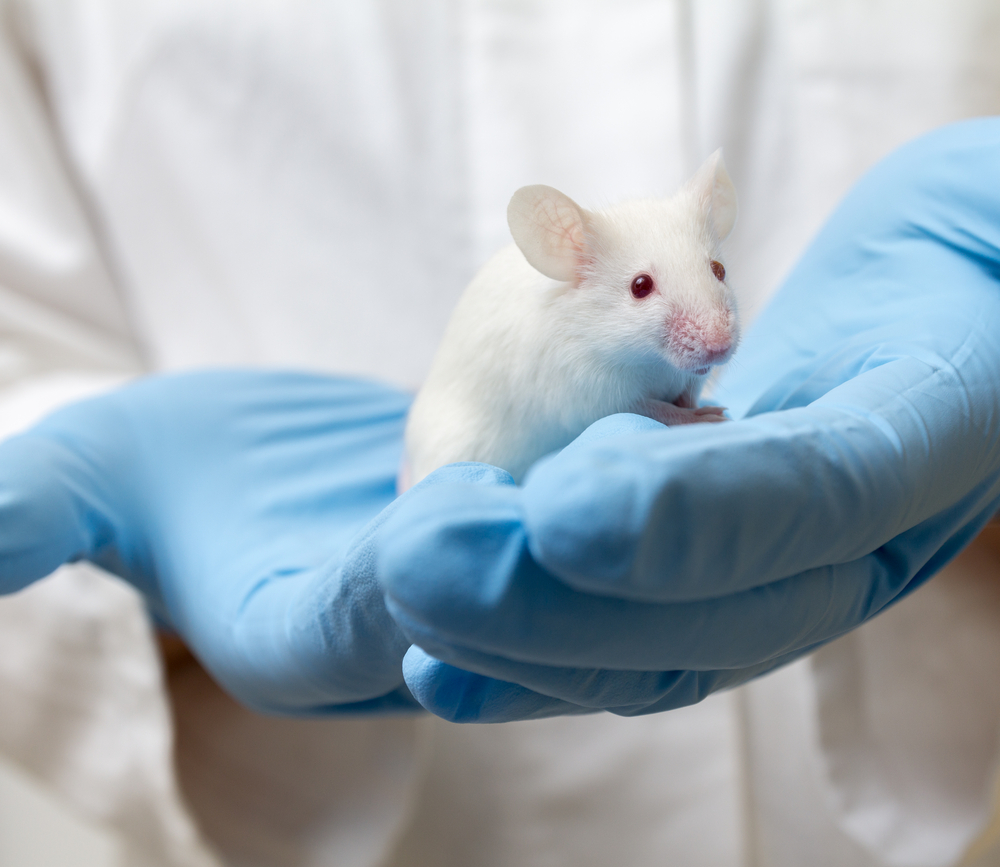
The investigators had previously developed neural progenitor cells — a kind of stem cell that can develop into neurons — from iPSCs generated using wild-type monkeys or monkeys with Huntington’s disease.
To “fix” the Huntington’s stem cells, the researchers used small-hairpin RNA (shRNA). Basically, this reduces the amount of mutant protein the cells make by decreasing the amount of messenger RNA the cell transcribes for a specific gene — in this case, huntingtin. This technique, unlike other gene-editing technologies such as CRISPR, has the advantage of not actually changing the cells’ genome, minimizing the chance for problematic off-target effects.
Mice with Huntington’s disease were surgically implanted (via an injection directly into the brain) with stem cells from both wild-type and Huntington’s monkeys and included cells that had and had not been modified with shRNA, as well as sham injections as a control.
Injection with both wild-type stem cells and modified cells from Huntington’s monkeys significantly elongated the survival time of mice, as well as improving traits such as grip strength. Molecular and imaging studies confirmed that the shRNA decreased the level of huntingtin produced and that the cells were growing into neurons in the mice’s brains.
“To our knowledge, no other studies have reported the combination of RNAi and neural progenitor stem cell therapy in [Huntington’s disease],” the researchers said. “We have demonstrated that the combination of gene and stem cell therapy can ameliorate HD symptoms in HD mice.”
Further research will be needed before such therapy is available for humans, but this study shows that, at least conceptually, iPSCs can be modified to help treat genetic diseases like Huntington’s.