Link Between Low Cysteine and Huntington’s Disease Revealed in Mouse Study
Researchers at Johns Hopkins University School of Medicine have found that patients with Huntington’s disease have a deficient system controlling the amount of the amino acid cysteine that goes inside cells — a deficit linked to oxidative stress.
The authors of the study, “Transcriptional control of amino acid homeostasis is disrupted in Huntington’s disease,” published in the journal Proceedings of the National Academy of Sciences, caution against self-medicating with cysteine supplements, stating that more research is needed to understand the role this nutrient plays in the body before it can be manipulated with treatments.
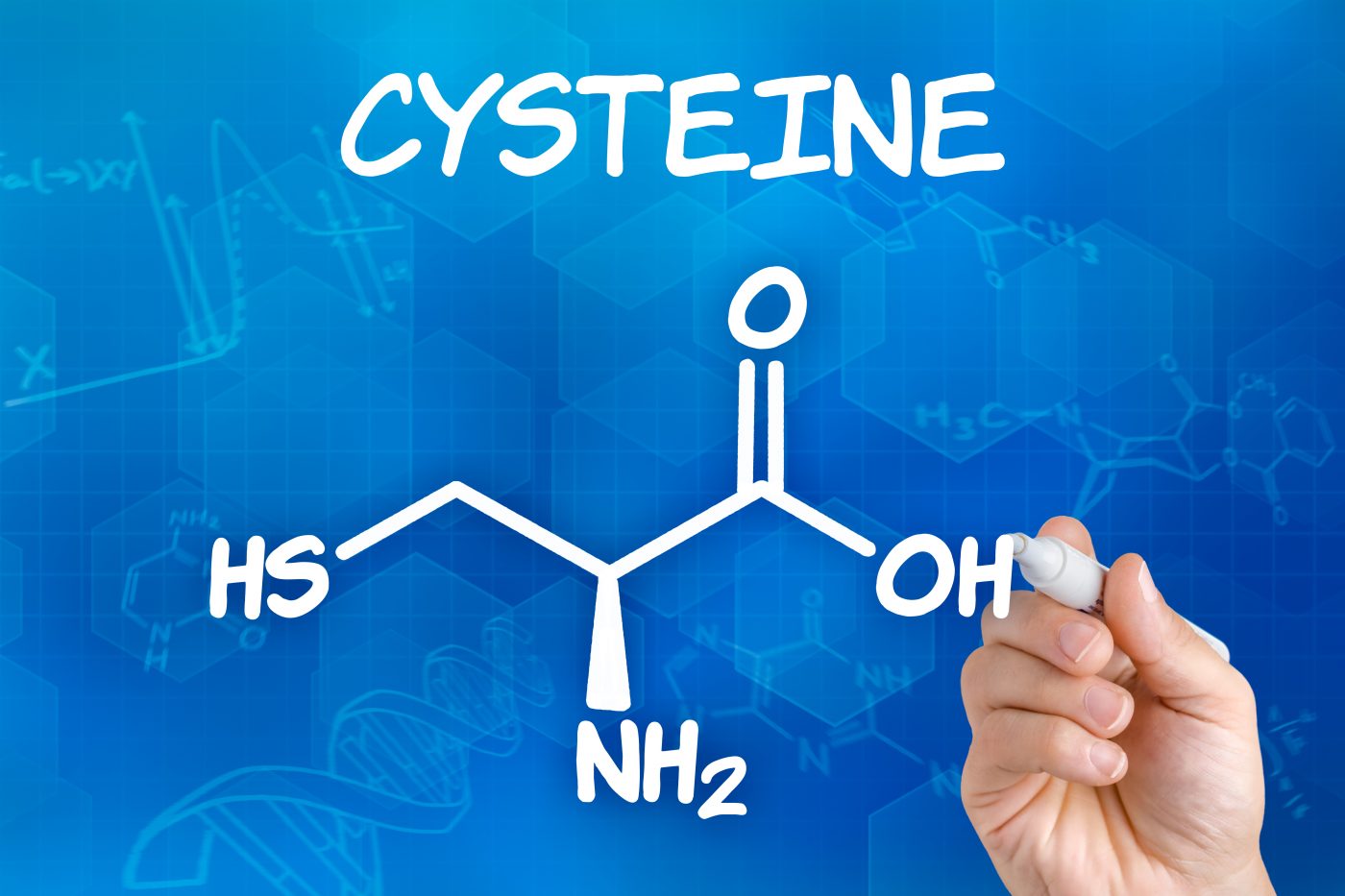
Scientists researching other diseases have noted that low levels of cysteine and high oxidative stress can be found in conditions as disparate as Alzheimer’s disease and AIDS. Senior study author Bindu Paul, PhD, realized that the amino acid plays a key role in controlling oxidative stress in cells, and figured that processes regulating both of these factors might also be involved in Huntington’s disease.
In 2014, Paul and her team published a study in the journal Nature showing that Huntington’s patients have low levels of the enzyme making cysteine, called CSE (cystathionine gamma-lyase). This enzyme is normally activated by a factor called ATF4 (activating transcription factor 4) when levels of the amino acid in the cell start running low, effectively telling the cell to ramp up production.
In addition to its use as a building block for proteins, this amino acid is crucial to protect cells against damage from oxidative stress. When cellular cysteine reserves get low, a cell can use alternative strategies to protect itself for a short time, but eventually, the oxidative damage becomes too much and the cell dies.
The team grew mouse neurons from both healthy and Huntington’s disease mice. When removing cysteine, healthy cells increased their ATF4 activity, just as expected. The cells from mice models of Huntington’s disease, however, did not produce ATF4 at all. This also turned out to be an effect limited to cysteine since depletion of other amino acids did not change the levels of ATF4.
“That intrigued us, and we wondered if elevated oxidative stress would affect the response of ATF4 because of cysteine’s role in cellular defense,” Paul said in a news release.
The team tested the idea by exposing the cells to the strong oxidant hydrogen peroxide. When removing cells’ cysteine source they could only produce small amounts of ATF4. When researchers, instead, treated cells from Huntington’s mice with the antioxidant vitamin C, the ability to produce ATF4 was rescued, and cells could again produce the amino acid.
“These findings implicate a vicious cycle where low levels of cysteine cause oxidative stress, which leads to decreased cysteine levels, therefore creating more oxidative stress, further slowing cysteine production,” said first study author Juan Sbodio, PhD.
The team’s previous work showed that spiking the diet of Huntington’s mice with cysteine improved symptoms, and while antioxidants are also known to improve symptoms in lab animals, the researchers state that it is too early to conclude that supplements might be beneficial in human patients.
In fact, too much cysteine can be toxic, and patients should always consult their physician before starting any supplement use.